ABA Therapy: Navigating Insurance Coverage
Written by the HeyASD Editorial Team
Navigating insurance coverage for ABA therapy can be a daunting task for families. ABA therapy is a crucial treatment for children with autism, and understanding how to secure insurance coverage is essential. This guide aims to simplify the process, helping families understand their policies, seek necessary authorizations, and maximize their benefits.
Key Takeaways
- Review your insurance policy thoroughly to understand ABA coverage specifics.
- State mandates can significantly impact your ABA therapy coverage.
- Pre-authorization is often required before starting ABA therapy.
- Working with insurance advocates and ABA providers can simplify the process.
- Appealing denied claims is possible and sometimes necessary.
Understanding ABA Therapy and Its Importance
What is ABA Therapy?
ABA Therapy, or Applied Behavior Analysis, is a scientific approach that helps children with autism learn and grow. It uses positive reinforcement to teach new skills and reduce unwanted behaviors. ABA therapy is highly adaptable, making it suitable for each child's unique needs.
Benefits of ABA Therapy for Children with Autism
ABA therapy offers numerous benefits for children with autism. It helps improve communication, social skills, and daily living activities. Families often find immense value in ABA therapy as it enhances essential life skills. This therapy not only supports the child but also provides practical strategies for the entire family to create a supportive environment.
Common Misconceptions About ABA Therapy
There are several misconceptions about ABA therapy. Some people think it's only about controlling behavior, but it's much more than that. ABA therapy focuses on teaching and reinforcing positive behaviors while reducing challenging ones. It's a holistic approach that aims to help children reach their fullest potential.
Reviewing Your Insurance Policy for ABA Coverage

Key Terms to Know in Your Insurance Policy
Before diving into your insurance policy, familiarize yourself with key terms. Understanding these terms can help you better navigate your coverage. Look for terms like deductible, co-pay, out-of-pocket maximum, and pre-authorization. Knowing these can make a big difference in understanding your benefits.
Steps to Review Your Policy
- Gather Your Documents: Collect your insurance policy documents. These can usually be found online or in physical form.
- Identify Relevant Sections: Look for sections related to behavioral health, autism spectrum disorders (ASD), or ABA therapy.
- Check for Limitations: Pay attention to any limitations, exclusions, or prerequisites for pre-authorization.
- Contact Your Provider: If anything is unclear, don't hesitate to contact your insurance provider for clarification.
Questions to Ask Your Insurance Provider
When speaking with your insurance provider, ask these important questions:
- Does my policy cover ABA therapy?
- Are there any limitations or exclusions?
- What is the process for obtaining pre-authorization?
- Are there any in-network providers I should use?
Taking the time to thoroughly review your insurance policy can save you a lot of headaches down the road. It ensures you know exactly what is covered and what steps you need to take to get the most out of your benefits.
State Mandates and Regulations for ABA Coverage
Overview of State Mandates
ABA therapy is covered by insurance in many states because mandates have been passed through the state legislature. All 50 U.S. states now have either a state mandate or a directive to cover ABA therapy. Fully-funded insurance policies are subject to these state mandates. Your state’s mandate may include other benefits such as speech therapy, occupational therapy, or physical therapy.
How State Regulations Affect Coverage
For families navigating autism support, understanding your state’s stance on ABA therapy coverage is crucial. While some states have comprehensive mandates requiring insurers to include ABA therapy for individuals with autism, others may offer more limited coverage or have specific criteria.
Finding State-Specific Information
Medicaid’s role in covering ABA therapy also varies, with some states providing broad support under this program. To get a clear picture of your state’s specific guidelines, you may want to conduct targeted research or speak with a knowledgeable ABA provider or insurance specialist in your region.
Seeking Pre-Authorization for ABA Therapy
What is Pre-Authorization?
Pre-authorization is a process where your insurance company reviews and approves the medical necessity of ABA therapy before you can start treatment. This step is crucial to ensure that your insurance will cover the therapy costs.
Steps to Obtain Pre-Authorization
- Consult Your Healthcare Provider: Work with your healthcare provider or an ABA specialist to gather all necessary documents.
- Submit Required Documentation: This typically includes diagnostic reports, a detailed treatment plan, and assessment scores.
- Wait for Approval: The insurance company will review the submitted documents and decide whether to approve the therapy.
Common Challenges and Solutions
- Incomplete Documentation: Ensure all required documents are complete and accurate to avoid delays.
- Denial of Pre-Authorization: If denied, ask for specific reasons and address them in a re-submission.
- Long Waiting Periods: Follow up regularly with your insurance provider to expedite the process.
Navigating the pre-authorization process can be challenging, but with persistence and the right support, you can secure the necessary coverage for ABA therapy. For more resources, consider visiting an autism store for additional support materials.
Working with Insurance Advocates and ABA Providers
Navigating insurance coverage for ABA therapy can be tricky, but families don't have to do it alone. Experts like insurance advocates or ABA providers who know how to deal with insurance companies can be a big help. These experts can give valuable tips, help families understand their rights, and assist in getting the most out of insurance benefits. They can also help families get the right paperwork ready, like treatment plans or medical records.
Maximizing Your Insurance Benefits
Understanding Your Rights and Entitlements
Knowing your rights under your insurance plan is crucial. Familiarize yourself with the benefits available to you, including any state mandates that may apply. This knowledge empowers you to advocate effectively for your child's needs.
Preparing Necessary Documentation
Having the right paperwork can make a big difference. Ensure you have treatment plans, medical necessity letters, and any other required documents ready. These can support your claims and appeals, making the process smoother.
Strategies for Maximizing Coverage
- Early Intervention: Many insurance plans emphasize the importance of starting therapy early. Aligning early intervention with your coverage can optimize your child's developmental outcomes.
- Utilization Reviews: Regularly review your insurance utilization to ensure you're making the most of your benefits. This can help you identify any gaps or areas for improvement.
- In-Network Providers: Choosing in-network providers can significantly reduce costs. Confirm that your preferred therapists are in-network to avoid unexpected expenses.
Being proactive in advocating for your child's needs ensures that families can fully utilize their insurance coverage and provide the best possible support and care.
Appealing Denied Claims for ABA Therapy
Reasons for Claim Denials
Insurance claims for ABA therapy can be denied for various reasons. Common reasons include missing documentation, lack of pre-authorization, or the insurer deeming the therapy not medically necessary. Understanding why your claim was denied is the first step in the appeal process.
Steps to Appeal a Denied Claim
- Review the Denial Letter: Carefully read the denial letter to understand the specific reasons for the denial.
- Gather Documentation: Collect all necessary documents, including medical records, treatment plans, and letters from your ABA provider.
- Write an Appeal Letter: Draft a compelling appeal letter that addresses the reasons for denial and includes supporting evidence.
- Submit Your Appeal: Send your appeal letter and documentation to your insurance company within the specified timeframe.
- Follow Up: Regularly check the status of your appeal and be prepared to provide additional information if needed.
Resources for Assistance
If you find the appeal process overwhelming, there are resources available to help. Insurance advocates and ABA providers can offer valuable support. They can help you navigate the process, gather necessary evidence, and present a strong case for the necessity of ABA therapy.
Don't lose hope if your insurance denies coverage for ABA treatment. You have the right to appeal this decision. Enlist the support of your ABA provider to help navigate the appeals process. They can help gather essential evidence and information to present a compelling case for the necessity of ABA therapy.
Finding In-Network ABA Providers
Importance of In-Network Providers
Choosing an in-network ABA provider can save you money. In-network providers have agreed-upon rates with your insurance company, which means lower out-of-pocket costs for you. This can make a big difference in managing the expenses of ABA therapy.
How to Find In-Network Providers
- Check Your Insurance Website: Most insurance companies have a list of in-network providers on their website. This is a good place to start.
- Call Your Insurance Company: If you can't find the information online, call your insurance company. They can tell you which providers are in-network.
- Ask Your ABA Provider: Some ABA providers can help you find out if they are in-network with your insurance.
Questions to Ask Potential Providers
When you find a potential ABA provider, ask these questions to make sure they are a good fit:
- Are you in-network with my insurance?
- What are your qualifications and certifications?
- What therapy settings do you offer?
- How do you tailor therapy to each child's needs?
Finding the right ABA provider is crucial for effective therapy. Make sure to do your research and ask the right questions to ensure the best care for your child.
Utilizing Expert Guidance for Benefits Verification
Navigating insurance coverage for ABA therapy can be tricky, but you don't have to do it alone. Experts can provide valuable insights and help you understand your rights and entitlements. They can also assist in maximizing your insurance benefits.
Role of Benefits Verification Experts
Benefits verification experts, like those at Behavior Frontiers, can contact your insurance company to gather precise details about your coverage. They will uncover crucial information such as copayments, deductibles, and whether pre-authorization is necessary.
How to Access Expert Guidance
You can seek guidance from healthcare providers who specialize in autism or ABA therapy. They can answer questions and help you understand the specific requirements and processes involved. Consulting with these experts ensures you get accurate information throughout your insurance coverage journey.
Benefits of Professional Assistance
Working with experts can be immensely helpful. They can help you prepare necessary documentation, such as treatment plans or medical necessity letters, to support insurance claims and appeals if needed. This assistance can make a significant difference in navigating the complexities of insurance coverage for ABA therapy.
Navigating Coverage Differences Across States
Understanding Coverage Variations
The landscape of ABA therapy coverage can shift dramatically as you cross state lines. Different states have unique mandates and regulations that impact whether and how much of ABA therapy is covered by insurance. Understanding these variations is crucial for ensuring your child receives the necessary care.
Tips for Families Moving Between States
- Research State Mandates: Before moving, research the specific ABA therapy coverage mandates in your new state.
- Update Your Insurance Provider: Inform your insurance company about your move to understand how your coverage will change.
- Consult Local Experts: Reach out to local autism support groups or ABA providers for insights on navigating the new state's insurance landscape.
Resources for State-Specific Information
Finding accurate, state-specific information can be challenging. Utilize resources like state health department websites, autism advocacy organizations, and insurance company customer service lines to gather the necessary details. Staying informed will help you make the best decisions for your child's care.
Navigating insurance coverage for ABA therapy can be complex, but with the right information and support, you can ensure your child gets the care they need.
Understanding the Financial Aspects of ABA Therapy
Cost of ABA Therapy
ABA therapy can be a significant financial commitment for families. The cost varies based on the intensity and duration of the therapy. On average, families might spend thousands of dollars annually. Understanding these costs upfront can help in planning and budgeting effectively.
Insurance vs. Out-of-Pocket Costs
When it comes to paying for ABA therapy, families often face a choice between using insurance or paying out-of-pocket. Insurance can cover a substantial portion, but out-of-pocket expenses can still be high. It's crucial to review your coverage details to know what is included and what isn't.
Financial Assistance Options
There are several financial assistance options available to help families manage the cost of ABA therapy. These include grants, scholarships, and state-funded programs. Exploring these options can provide much-needed relief and ensure that children receive the therapy they need.
Navigating the financial aspects of ABA therapy can be challenging, but with the right information and resources, families can find ways to make it more affordable.
Conclusion
Navigating insurance coverage for ABA therapy can seem like a daunting task, but with the right approach, it becomes manageable. By thoroughly reviewing your insurance policy, seeking help from experts, and staying persistent, you can secure the necessary coverage for your child's therapy. Remember, each insurance plan is different, so understanding your specific benefits is crucial. With patience and determination, you can ensure that your child receives the essential ABA services they need to thrive.
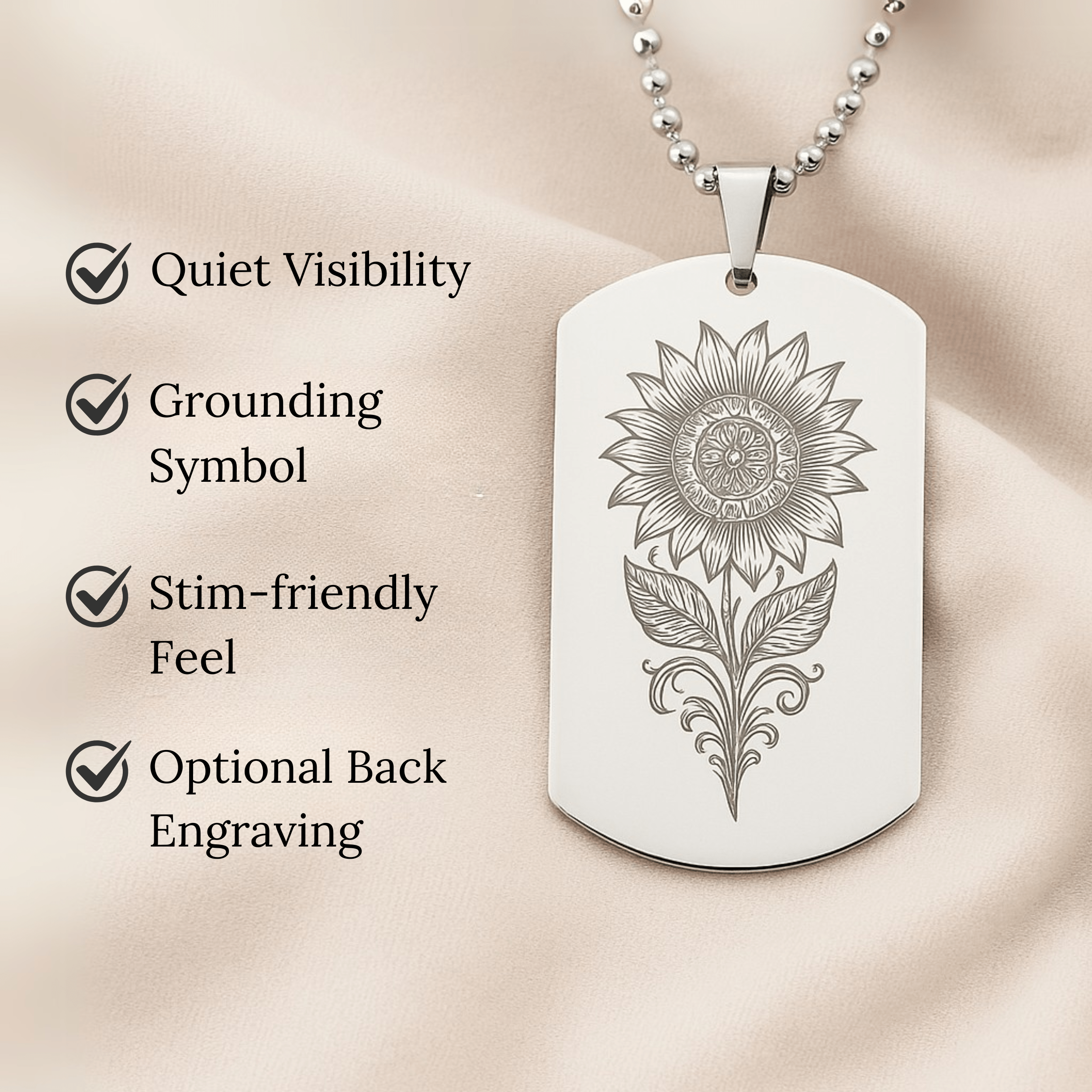
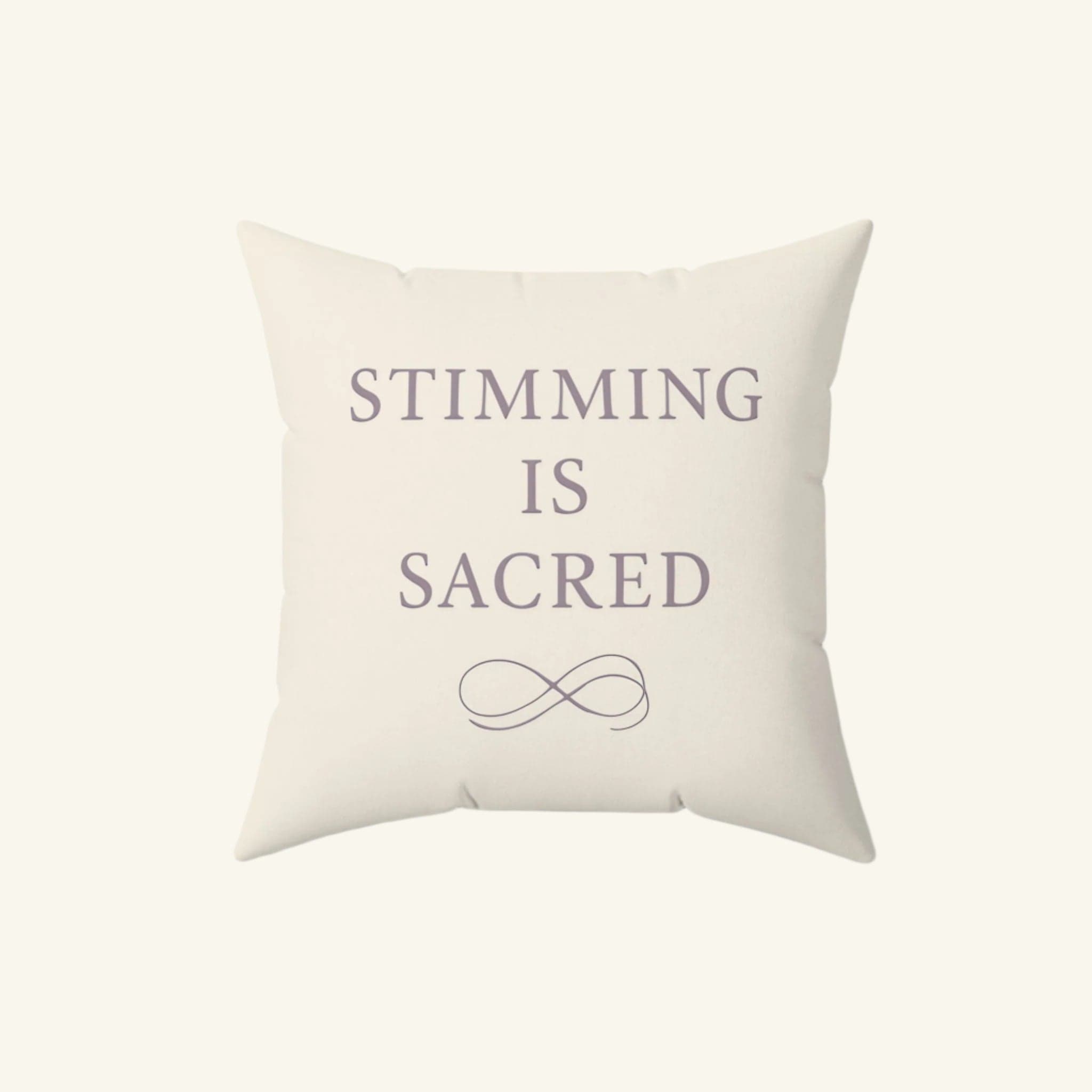
Join Hundreds of Autistic Adults Feeling
More Comfort in Their Own Skin
Use code WELCOME10 for 10% off your first order.
Start Your Comfort JourneyFrequently Asked Questions
What is ABA therapy?
ABA therapy, or Applied Behavior Analysis, is a type of therapy that helps improve specific behaviors, such as social skills, communication, and learning skills, through reinforcement strategies.
Why is ABA therapy important for children with autism?
ABA therapy is important because it helps children with autism develop essential skills and reduce problematic behaviors, making it easier for them to interact with others and learn new things.
How can I find out if my insurance covers ABA therapy?
To find out if your insurance covers ABA therapy, review your insurance policy, contact your insurance provider, and ask specific questions about ABA therapy coverage.
What are state mandates for ABA therapy coverage?
State mandates are laws that require insurance companies to cover ABA therapy. These mandates vary by state, so it's important to check the specific regulations in your state.
What should I do if my insurance claim for ABA therapy is denied?
If your insurance claim is denied, you can appeal the decision. Start by understanding the reason for the denial, gather necessary documentation, and follow the steps outlined by your insurance provider for the appeals process.
How can ABA providers help with insurance coverage?
ABA providers can assist by helping you understand your insurance benefits, preparing necessary documentation, and working directly with your insurance company to ensure coverage for the therapy.
What is pre-authorization for ABA therapy?
Pre-authorization is a process where your insurance company reviews and approves the ABA therapy services before they begin. This ensures that the therapy will be covered under your insurance plan.
Are there financial assistance options for ABA therapy?
Yes, there are financial assistance options available, such as grants, scholarships, and state-funded programs, to help cover the costs of ABA therapy if insurance does not fully cover it.
On This Page
Frequently asked questions
How can I find out if my insurance plan includes ABA therapy insurance coverage for my child?
What steps should I take to get pre-authorization for ABA therapy through my insurance?
What should I do if my insurance denies coverage for ABA therapy or sensory-friendly therapy support?
How do state mandates affect the autism insurance coverage available to my family?
Are there sensory tools or calming blankets that can support my child alongside ABA therapy?
How can working with insurance advocates or ABA providers help me navigate disability insurance for autism?
What documentation do I need to prepare to maximize my insurance benefits for ABA therapy?
How can I find in-network ABA providers to reduce out-of-pocket costs?
Can Autism-themed decor or comfortable clothing like t-shirts help create a supportive environment for my child during therapy?
About the HeyASD Editorial Team
Autistic‑owned • Values‑led • Sensory‑friendly design
We are autistic creators, writers, and advocates dedicated to producing resources that are practical, sensory-aware, and grounded in lived experience. Our mission is to make information and products that support the autistic community accessible to everyone, without jargon or condescension. Learn more about our team.
This article is written from lived autistic experience and an evidence-aware perspective. It is for general informational purposes only and should not be taken as medical, legal or therapeutic advice.
Always consult a qualified clinician or occupational therapist for individual needs and circumstances.
About Our Autism Blog
HeyASD isn’t just a store, it’s a calm, supportive space created by and for autistic adults. Our blog shares sensory-friendly tips, identity-affirming stories, and heartfelt resources for navigating life as an autistic person. Whether you're late-diagnosed, exploring your needs, or supporting someone you love, you're welcome here.
Thank you for reading. We hope these resources bring comfort and clarity.