Autism Research and Immune System Implications
Written by the HeyASD Editorial Team
Autism Spectrum Disorder (ASD) is a complex condition that affects how a person thinks, interacts, and experiences the world. Scientists are exploring how the immune system might play a role in ASD. This article looks at how the immune system and autism are connected, from genetic links to environmental factors.
Key Takeaways
- The immune system might be linked to autism through genes and environmental factors.
- Researchers are studying how immune system problems could affect brain development in autism.
- Some studies suggest that infections during pregnancy might increase the risk of autism.
- There is evidence that gut bacteria and the immune system could influence autism symptoms.
- New treatments targeting the immune system are being explored for autism.
The Role of the Immune System in Autism
Historical Perspectives on Immune System Research
Nearly 50 years ago, researchers noticed a link between autism and congenital rubella infection. Since then, many other infections have been connected to autism. Mounting evidence shows that the immune system and its abnormal functions, like inflammation and cytokine dysregulation, can significantly influence autism. This has led scientists to explore the role of immune dysregulation and autoimmunity in autism.
Key Immune System Components Involved in Autism
The immune system is complex, involving many cells and molecules. In autism, several components are often altered:
- Cytokines: These are signaling molecules that help regulate the immune response. In autism, cytokine levels can be imbalanced.
- Anti-brain autoantibodies: These are antibodies that mistakenly target the brain, potentially affecting neurodevelopment.
- Natural Killer (NK) Cells: These cells are part of the body's first line of defense. In autism, NK cells may show increased baseline activity but decreased response to activation.
Current Understanding of Immune Dysregulation
Today, we know that immune dysregulation plays a role in autism. This includes an increased pro-inflammatory environment and altered immune cell populations. For example, T-cell and NK-cell populations may be skewed, leading to a shift in cell subpopulations. This ongoing immune dysregulation can persist from birth through childhood, affecting behavior and development.
Understanding the role of the immune system in autism opens new avenues for potential treatments and interventions.
Genetic Links Between Autism and Immune Function
Genetic Studies Highlighting Immune System Genes
Research has shown that many genes linked to autism are also involved in the immune system. For example, a 2014 study found that the majority of genetic risk for autism comes from common variations, many of which are related to immune function. This suggests a strong genetic connection between autism and immune system regulation.
Common Genetic Pathways in Autism and Immune Disorders
Several studies have identified common genetic pathways that are involved in both autism and immune disorders. These pathways often include genes related to cytokine signaling and natural killer (NK) cell function. The overlap in these pathways indicates that immune dysregulation may play a significant role in the development of autism.
Implications for Future Genetic Research
Understanding the genetic links between autism and the immune system can open new avenues for research and treatment. Future studies could focus on identifying specific genetic markers that contribute to both conditions. This could lead to the development of targeted therapies that address both autism symptoms and immune system dysfunction.
The exploration of genetic links between autism and immune function is crucial for developing new treatments and improving the quality of life for individuals with autism.
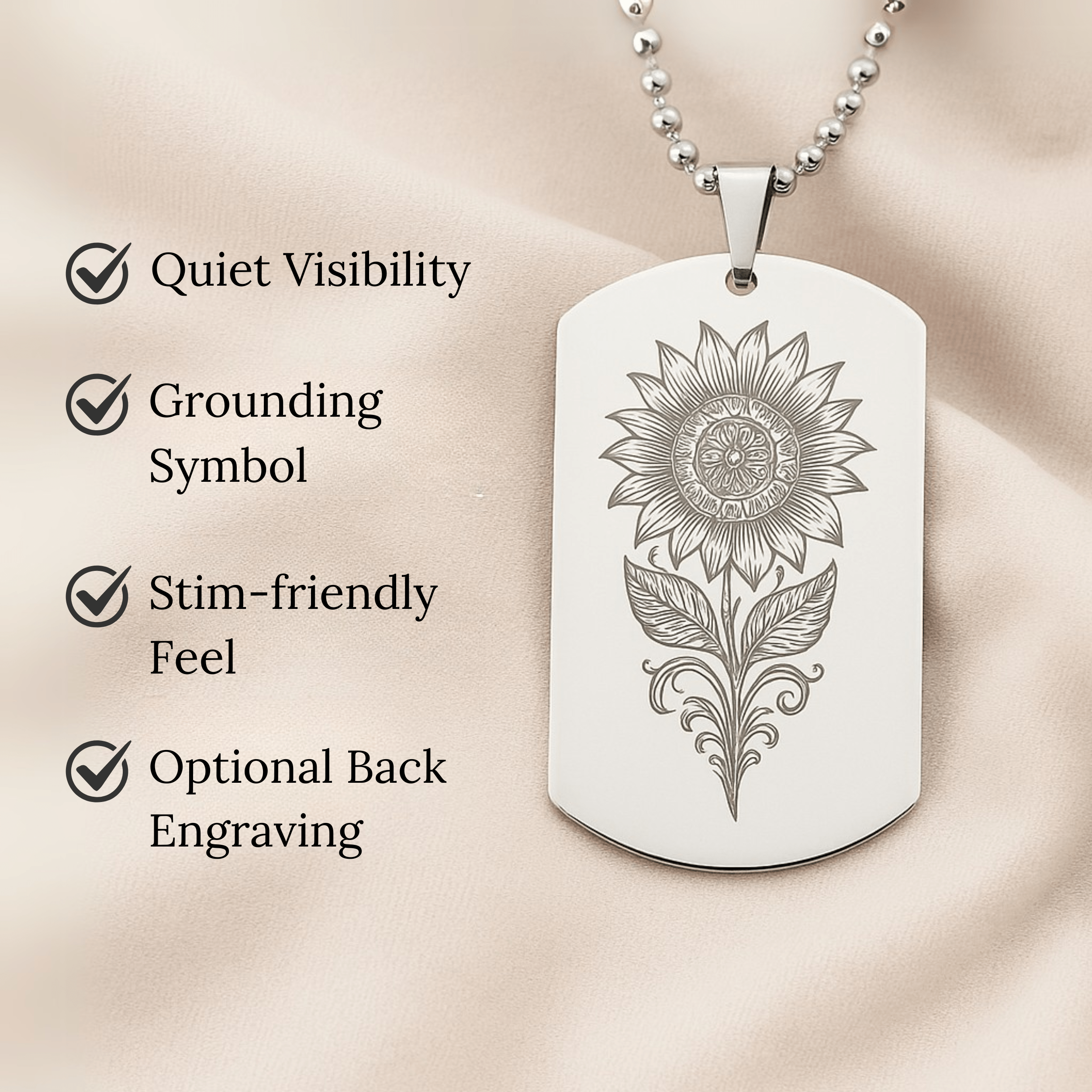
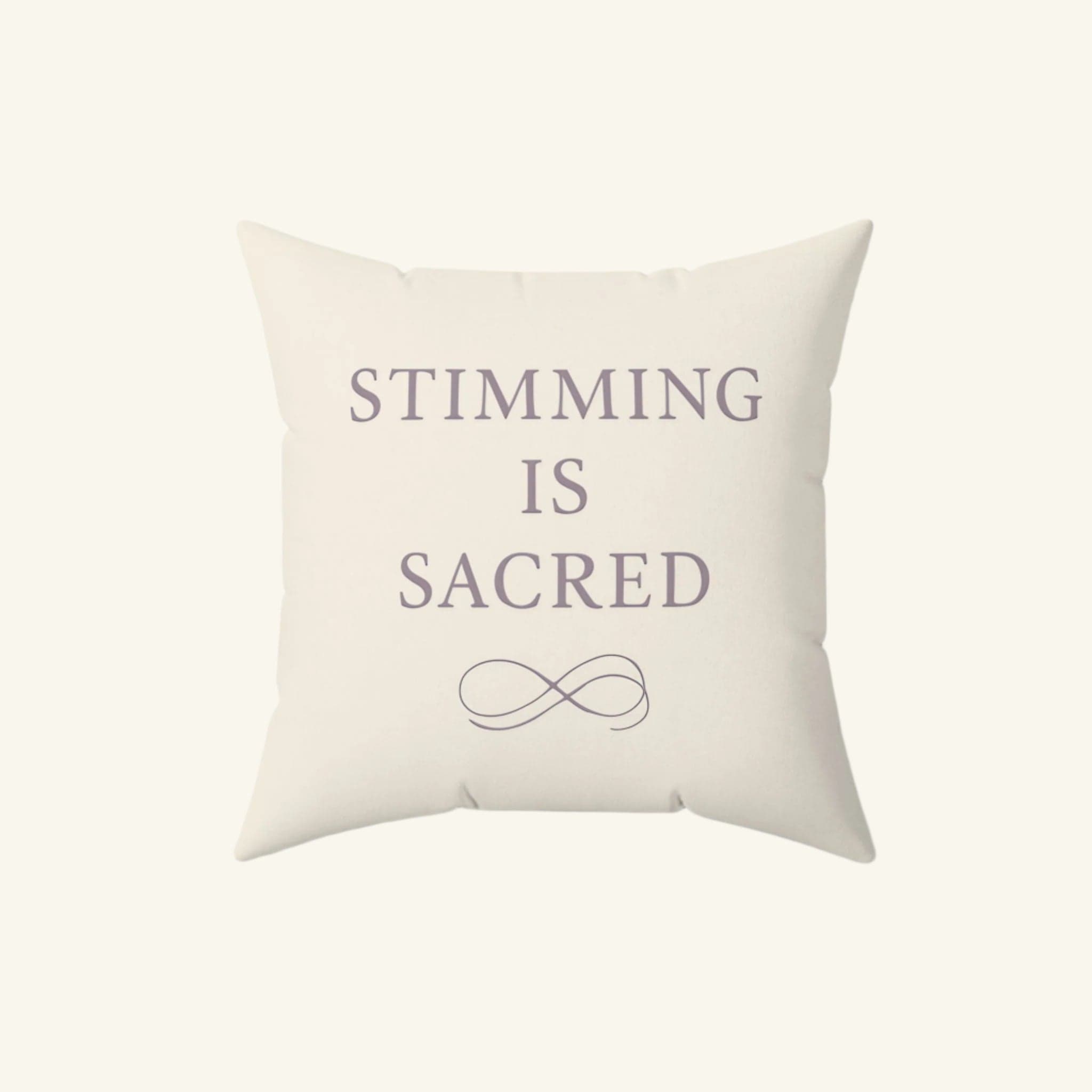
Explore a variety of autism-themed products including t-shirts, wall art, jigsaw puzzles, hats, and journals. Each item aims to celebrate individuality and raise awareness about autism. Enjoy free shipping on orders over $49 and find unique ways to express support for the autism community.
Prenatal Factors Influencing Autism and Immune Function
Maternal Infections and Immune Activation
Nearly 50 years ago, researchers noticed a link between autism and congenital rubella infection. Since then, many other infections have been connected to autism. Maternal infections during pregnancy can trigger the mother's immune system, which might affect the baby's brain development. This immune response, even without an actual infection, can lead to changes in the child's brain.
Impact of Maternal Autoantibodies
Some mothers have autoantibodies that target the baby's brain. These autoantibodies can interfere with normal brain development, increasing the risk of autism. Studies show that about 20% of mothers with autistic children have these autoantibodies.
Role of Pro-inflammatory Cytokines
Pro-inflammatory cytokines are chemicals that the immune system uses to communicate. High levels of these cytokines in the mother can affect the baby's brain development. This inflammation can lead to changes in the brain that are linked to autism.
Understanding how the immune system affects brain development can help us find new ways to prevent and treat autism.
Postnatal Immune Dysregulation in Autism
Systemic Inflammation in Children with Autism
Children with autism often show signs of systemic inflammation. This includes higher levels of inflammatory cytokines like IL-6 and IL-8. These cytokines can lead to a pro-inflammatory environment, which may affect brain development and behavior.
Anti-brain Autoantibodies and Neurodevelopment
Some children with autism have their own anti-brain autoantibodies. These are different from maternal antibodies and are linked to unusual behaviors and developmental issues. These autoantibodies can interfere with normal brain function.
Environmental Triggers of Immune Dysregulation
Various environmental factors can trigger immune dysregulation in children with autism. These include exposure to toxins, infections, and even certain foods. Understanding these triggers can help in managing symptoms and improving quality of life.
The ongoing immune dysregulation in autism is a complex issue that requires a deeper understanding of both genetic and environmental factors.
Gut Microbiota and Immune System Interactions in Autism
Gut-Brain Axis and Autism
The gut-brain axis is a complex communication network linking the gut and the brain. Research shows that this connection plays a significant role in autism. The gut microbiota can influence brain function and behavior through immune, neural, and hormonal pathways.
Microbiota Composition in Autistic Individuals
Studies have found that individuals with autism often have different gut microbiota compositions compared to neurotypical individuals. These differences can affect the immune system and may contribute to autism symptoms. For example, some autistic individuals have higher levels of certain bacteria that produce pro-inflammatory compounds.
Therapeutic Potential of Modulating Gut Microbiota
Modulating the gut microbiota offers a promising therapeutic approach for autism. Probiotics, prebiotics, and dietary changes can help balance the gut microbiota, potentially improving both gut health and behavioral symptoms. Ongoing research aims to identify the most effective strategies for modulating the gut microbiota in autistic individuals.
Understanding the gut-brain axis and its impact on autism could lead to new, more effective treatments for those affected by the condition.
Autoimmunity and Autism Spectrum Disorders
Autoimmune Diseases Co-occurring with Autism
Research has shown a link between autism and autoimmune diseases. Some scientists even suggest that autism might be an autoimmune disorder. Children of mothers with autoimmune diseases like lupus have a higher risk of autism. This connection is especially significant because it highlights the role of the immune system in autism.
Mechanisms of Autoimmune Responses in Autism
Autoimmune responses in autism may be triggered by environmental factors like viruses. These triggers can cause the immune system to attack the brain, leading to autism symptoms. Anti-brain autoantibodies, which are found in other autoimmune diseases, are also present in some autistic individuals. This suggests a shared mechanism between autism and other autoimmune disorders.
Potential for Immunomodulatory Therapies
Given the link between autoimmunity and autism, immunomodulatory therapies could be a promising treatment. These therapies aim to regulate the immune system and reduce inflammation. By targeting the immune system, we might improve the quality of life for autistic individuals. This approach is still in the early stages, but it offers hope for future treatments.
Understanding the role of the immune system in autism could lead to new, effective treatments.
For more information on how therapies can improve the quality of life for autistic individuals, visit the autism store.
Cytokine Profiles in Autism
Elevated Pro-inflammatory Cytokines
Research shows that children with autism often have higher levels of pro-inflammatory cytokines. These are chemicals that help the immune system respond to threats. High levels of these cytokines can lead to inflammation, which might affect brain development. For example, studies found increased levels of IL-1β, IL-6, and TNF-α in children with autism.
Cytokine Imbalances and Behavioral Symptoms
Cytokine imbalances are linked to behavioral symptoms in autism. When the balance between pro-inflammatory and anti-inflammatory cytokines is off, it can lead to issues like visual stimming. This imbalance might also affect social interactions and communication skills. Researchers are still exploring how these imbalances directly impact behavior.
Research on Cytokine-targeted Treatments
Scientists are looking into treatments that target cytokines to help manage autism symptoms. These treatments aim to reduce inflammation and restore balance in the immune system. Some early studies show promise, but more research is needed to confirm their effectiveness.
Understanding cytokine profiles in autism could lead to better treatments and improved quality of life for those affected.
Immunogenetic Factors in Autism

Key Immunogenetic Markers Identified
Research has shown a link between certain HLA alleles and autism. For example, the DRB1*0401 allele is associated with a higher risk of autism in children from various populations, including Utah and Han Chinese. HLA-DR4 is another marker that appears more frequently in children with autism and their mothers.
Natural Killer Cells and Cytokine Regulation
Natural killer (NK) cells play a crucial role in the immune system. In individuals with autism, NK cells may not function properly, leading to immune dysregulation. This can result in an imbalance of cytokines, which are proteins that help regulate the immune response. Elevated levels of pro-inflammatory cytokines have been observed in autistic individuals.
Future Directions in Immunogenetic Research
Future research aims to explore the complex relationship between genetics and the immune system in autism. Understanding these connections could lead to new diagnostic tools and treatments. The goal is to develop personalized medicine approaches that consider an individual's unique genetic and immunological profile.
The interplay between genetics and the immune system in autism is a promising area of research that could lead to significant advancements in diagnosis and treatment.
Clinical Implications of Immune System Research in Autism
Diagnostic Tools for Immune Dysregulation
Understanding the immune system's role in autism can lead to better diagnostic tools. Identifying immune markers could help in early detection and personalized treatment plans. This approach may also aid in distinguishing between different autism subtypes, making treatments more effective.
Personalized Medicine Approaches
Personalized medicine tailors treatments to individual needs. By focusing on immune system differences, doctors can create specific therapies for each person. This method promises more effective and targeted treatments, improving overall outcomes for those with autism.
Challenges and Opportunities in Treatment
While the link between autism and the immune system is promising, it comes with challenges. The variety of symptoms and co-existing conditions makes it hard to develop one-size-fits-all treatments. However, ongoing research offers hope for new therapies that could significantly improve the quality of life for individuals with autism.
The future of autism treatment lies in understanding the complex relationship between the immune system and neurodevelopment. This knowledge could pave the way for groundbreaking therapies and better support for those affected by autism.
Emerging Therapies Targeting Immune Dysfunction in Autism
Stem Cell Therapies and Immune Modulation
Stem cell therapies are showing promise in treating autism by addressing immune dysfunction. Stem cells can help repair damaged tissues and modulate the immune system. This approach aims to correct neurodevelopmental issues at a cellular level.
Nutritional Interventions for Immune Health
Diet plays a crucial role in managing immune health. Nutritional interventions, such as specific diets and supplements, can help reduce inflammation and improve overall well-being in autistic individuals. These interventions are tailored to meet the unique needs of each person.
Clinical Trials and Future Prospects
Ongoing clinical trials are exploring various therapies targeting immune dysfunction in autism. These trials aim to find effective treatments and improve the quality of life for those affected. The future looks promising as researchers continue to uncover new therapeutic options.
Neuroinflammation and Autism
Brain Inflammation in Autism
Neuroinflammation is a key area of study in autism research. Brain inflammation has been observed in many individuals with autism, suggesting a link between the immune system and neurodevelopmental disorders. Microglia, the brain's immune cells, often show increased activity in autistic individuals, indicating an ongoing inflammatory response.
Immune Signaling Pathways in the Brain
The brain's immune signaling pathways play a crucial role in neuroinflammation. Cytokines, which are signaling molecules, can influence brain function and behavior. Elevated levels of pro-inflammatory cytokines like IL-6 and TNF-alpha have been found in autistic individuals, pointing to a disrupted immune response.
Potential for Anti-inflammatory Treatments
Given the role of inflammation in autism, there is growing interest in anti-inflammatory treatments. These therapies aim to reduce brain inflammation and improve symptoms. Some studies have shown promising results, but more research is needed to fully understand their effectiveness.
Understanding the link between neuroinflammation and autism could open new avenues for treatment, offering hope for better management of the condition.
Exploring these immune system implications is crucial for developing targeted therapies that could significantly improve the quality of life for those with autism.
Environmental Influences on Immune Function and Autism
Impact of Environmental Toxins
Environmental toxins can play a significant role in the development of autism. Exposure to pollutants like heavy metals and pesticides has been linked to immune system changes that may contribute to autism. These toxins can disrupt normal immune responses, leading to chronic inflammation and other issues.
Dietary Factors and Immune Health
Diet is another crucial factor. Certain foods can either support or harm the immune system. For instance, a diet high in processed foods and low in nutrients can weaken immune function. On the other hand, a balanced diet rich in antioxidants and vitamins can help maintain a healthy immune system.
Preventive Strategies for At-risk Populations
Preventive strategies are essential for those at risk. These can include avoiding exposure to known toxins, maintaining a healthy diet, and regular medical check-ups. By taking these steps, we can potentially reduce the risk of immune dysregulation and its impact on autism.
Understanding the environmental factors that influence immune function is crucial for developing effective preventive strategies for autism.
Conclusion
In summary, the connection between autism and the immune system is becoming clearer with ongoing research. Scientists have found that many children with autism show changes in their immune systems, which might affect their behavior and development. This means that autism could be more than just a brain disorder; it might involve the whole body. Understanding these immune changes can help doctors find new ways to treat autism. As we learn more, we hope to improve the lives of those with autism by addressing these immune system issues.
Join Hundreds of Autistic Adults Feeling
More Comfort in Their Own Skin
Use code WELCOME10 for 10% off your first order.
Start Your Comfort JourneyFrequently Asked Questions
What is the connection between the immune system and autism?
Researchers have found that the immune system and autism might be linked. Some studies show that people with autism have differences in their immune system, like more inflammation and unusual immune responses.
How do genetic factors play a role in autism and immune function?
Certain genes that affect the immune system are also linked to autism. This means that changes in these genes might lead to both immune problems and autism in some people.
Can infections during pregnancy affect the risk of autism?
Yes, infections during pregnancy can influence the risk of autism. When a mother has an infection, her immune system gets activated, which might affect the baby's brain development.
How does the gut microbiota relate to autism?
The gut microbiota, which is the community of bacteria in our intestines, can impact the brain and immune system. Some studies suggest that people with autism have different gut bacteria, which might influence their symptoms.
Are there treatments targeting the immune system for autism?
Some treatments aim to help the immune system in people with autism. These include therapies like stem cell treatments, nutritional changes, and medications that reduce inflammation.
What are cytokines and how do they relate to autism?
Cytokines are proteins that help control the immune system. In people with autism, the levels of certain cytokines might be higher or lower, which can affect behavior and brain function.
Can environmental factors influence autism and the immune system?
Yes, environmental factors like pollution, diet, and exposure to toxins can impact both the immune system and the risk of autism. These factors can cause changes in how the immune system works.
What is the potential for future research on autism and the immune system?
Future research might find new ways to diagnose and treat autism by looking at the immune system. Scientists are exploring how immune-based therapies could help improve symptoms in people with autism.
On This Page
Frequently asked questions
How does current research explain the connection between the immune system and autism?
What are some common immune system changes seen in autistic individuals?
How might genetic factors link autism and immune system function?
In what ways can sensory processing differences in autism relate to immune dysregulation?
Are there sensory-friendly products or calming tools that can support immune and sensory needs in autism?
How do maternal infections and immune responses during pregnancy influence autism risk?
What role does neuroinflammation play in autism, and how might it affect behavior?
How can understanding immune system differences lead to more personalized autism treatments?
What types of autism-themed items, like clothing or decor, help raise awareness about the autism immune system connection?
About the HeyASD Editorial Team
Autistic‑owned • Values‑led • Sensory‑friendly design
We are autistic creators, writers, and advocates dedicated to producing resources that are practical, sensory-aware, and grounded in lived experience. Our mission is to make information and products that support the autistic community accessible to everyone, without jargon or condescension. Learn more about our team.
This article is written from lived autistic experience and an evidence-aware perspective. It is for general informational purposes only and should not be taken as medical, legal or therapeutic advice.
Always consult a qualified clinician or occupational therapist for individual needs and circumstances.
About Our Autism Blog
HeyASD isn’t just a store, it’s a calm, supportive space created by and for autistic adults. Our blog shares sensory-friendly tips, identity-affirming stories, and heartfelt resources for navigating life as an autistic person. Whether you're late-diagnosed, exploring your needs, or supporting someone you love, you're welcome here.
Thank you for reading. We hope these resources bring comfort and clarity.