The Gut-Brain Connection in Autism

Written by HeyASD.com Team
The intricate relationship between the gut microbiome and the brain is a significant area of study, especially in the context of Autism Spectrum Disorder (ASD). The gut-brain axis represents a complex communication network that can influence neurodevelopment and behavior. This article delves into the connections between gut dysbiosis, gastrointestinal issues, and ASD, highlighting the potential of dietary interventions and the role of the immune system in this dynamic interplay. It also explores the latest research findings and clinical perspectives on treating autism through the gut.
Key Takeaways
- The gut-brain axis is a bi-directional communication system that plays a pivotal role in neurodevelopment and behavioral outcomes in ASD.
- Gastrointestinal issues are prevalent in individuals with autism and can significantly impact their quality of life and behavioral patterns.
- Alterations in the gut microbiome, such as gut dysbiosis, are linked to ASD and can affect the central nervous system through various pathways.
- Dietary interventions, including prebiotics and probiotics, show promise in modifying the gut microbiome and potentially improving ASD symptoms.
- Emerging research and clinical practice are increasingly focusing on the gut microbiome as a target for intervention and personalized treatment in autism.
Exploring the Gut-Brain Axis in Autism
Defining the Gut-Brain Axis
The gut-brain axis represents a complex communication network that integrates the gastrointestinal system with the brain's intricate functions. This axis is crucial for maintaining overall health and plays a pivotal role in neurodevelopmental conditions, such as autism. Disruptions in this axis can lead to a range of gastrointestinal issues, which are prevalent among individuals with autism, affecting their well-being and behavior.
The bidirectional nature of the gut-brain axis means that not only does the brain influence gut health, but the gut also sends signals back to the brain. These signals can be biochemical, stemming from the gut microbiota, or neural, through the enteric nervous system. The gut's influence on the brain is mediated by various pathways, including immune responses and hormonal secretions, which can impact a person's mental state and behavior.
The gut-brain axis is a testament to the body's interconnectedness, where the state of the gut microbiome can reflect and influence neurological health.
Understanding the gut-brain axis in autism involves exploring how gut dysbiosis, or an imbalance in gut microbiota, can affect neurodevelopment and behavior. Research has identified several mechanisms through which the gut microbiota influences brain function, such as the modulation of the immune system, production of neuroactive compounds, and regulation of neurotransmitter systems.
The Bidirectional Communication Pathway
The gut-brain axis is a complex network where the gut and brain communicate, influencing each other's functions. This pathway is particularly intriguing in the context of autism, where dysfunctions in signaling can lead to neural imbalances. These imbalances are often characterized by a disruption in excitatory and inhibitory synapses, which are crucial for proper brain function.
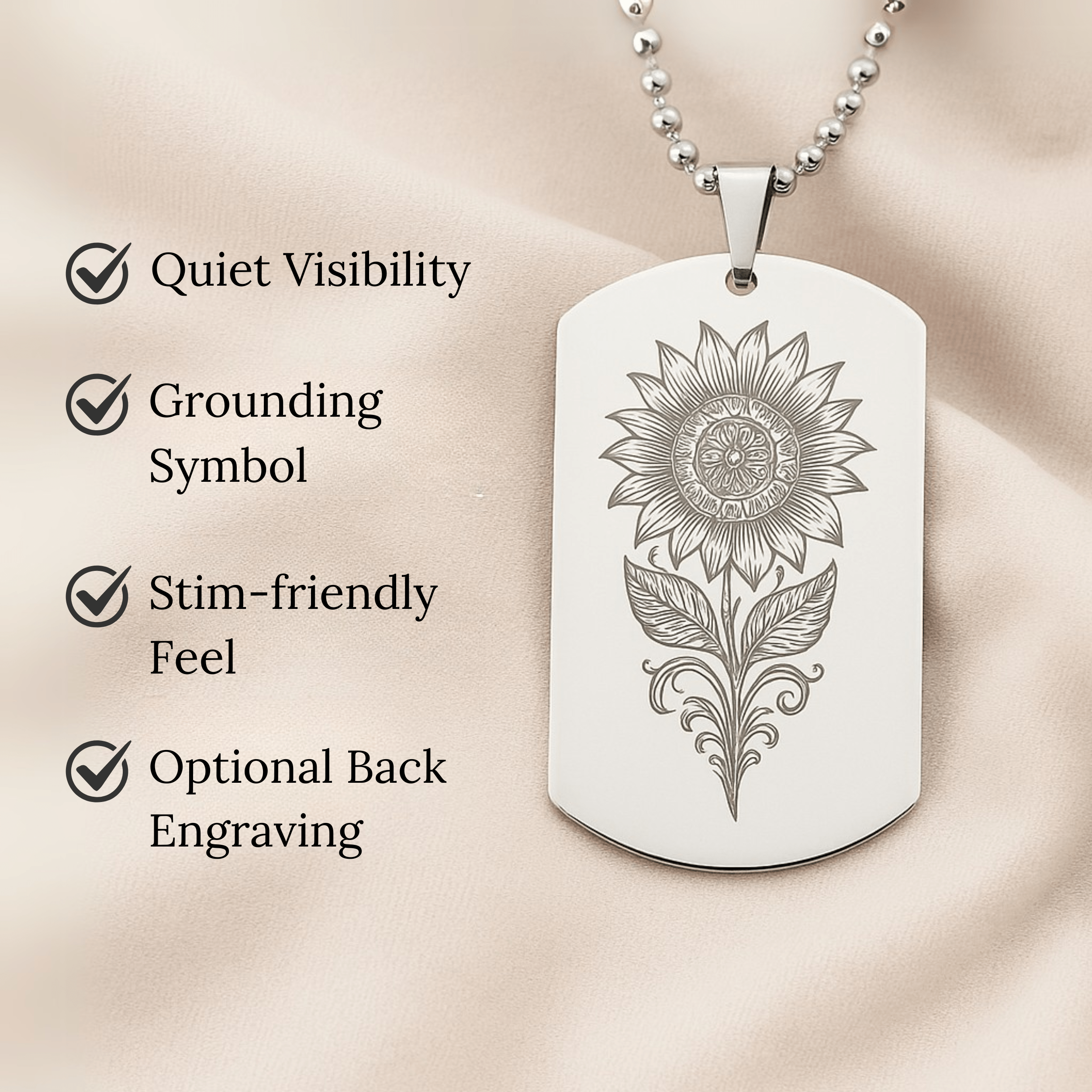
Autism store products often cater to sensory needs, such as visual stimming, which can be a response to these neural imbalances. The bidirectional nature of the gut-brain communication suggests that gut health could potentially influence behaviors associated with autism.
The maintenance of stable neural communication is essential for cognitive functions and social behavior, which are often areas of difficulty for individuals with autism.
Understanding this communication pathway opens up possibilities for targeted interventions, including dietary changes that may help to stabilize neural signaling and improve quality of life.
Implications for Neurodevelopment
The gut-brain axis is not just a fascinating scientific concept; it's a critical player in the unfolding story of neurodevelopment. Early life influences, such as the gut microbiota, can have profound effects on the brain's development. The Developmental Origins of Health and Disease (DOHaD) hypothesis underscores the vulnerability of infants' neurodevelopmental programming to a mix of genetic predisposition and environmental factors.
- Genetic predisposition
- Environmental triggers
- Neurodevelopmental programming
These elements can predispose individuals to enduring behavioral and cognitive changes, particularly in conditions like autism spectrum disorders (ASD). The gut microbiome's evolution during sensitive periods of brain development—when neurogenesis and synaptic rearrangement are most plastic—suggests that interventions targeting gut health could be pivotal.
The maintenance of stable neural communication is essential, relying on the proper construction of synapses and the balance of excitatory and inhibitory signals.
Understanding the biological mechanisms that link gut microbes with neurodevelopment is crucial. It paves the way for novel early therapeutic interventions aimed at mitigating the risks associated with neurodevelopmental disorders. The gut-brain connection opens a window to interventions that could reshape the trajectory of conditions like ASD, offering hope for more effective treatments.
Gastrointestinal Issues in Autistic Individuals
Prevalence of GI Disorders
The intersection of gastrointestinal (GI) disorders and autism spectrum disorder (ASD) is marked by a notable prevalence of GI symptoms among individuals with ASD. Studies consistently report a spectrum of GI issues, including constipation, diarrhea, and abdominal pain, which are more common in this population compared to neurotypical peers.
Gastrointestinal Severity Index (6-GSI) and the Questionnaire on Pediatric Gastrointestinal Symptoms-Rome III (QPGS-RIII) are among the tools used to assess these symptoms, underscoring the need for standardized evaluation methods. The presence of GI symptoms has been linked to the severity of ASD symptoms, suggesting a deep-rooted connection between gut health and neurodevelopmental outcomes.
The co-occurrence of GI disorders in individuals with ASD is not just a peripheral issue; it's a central aspect of their well-being that requires attention and care.
A closer look at the data reveals that GI symptoms are not just occasional occurrences but a persistent challenge for many with ASD. This underscores the importance of recognizing and addressing GI health as a key component of comprehensive autism care.
Impact on Quality of Life
The presence of gastrointestinal (GI) issues in individuals with autism spectrum disorder (ASD) can significantly diminish their quality of life. Chronic discomfort and pain associated with GI disorders often lead to heightened stress and anxiety, exacerbating behavioral challenges. The social implications are profound, as discomfort can hinder participation in educational settings and social interactions, further isolating individuals with ASD.
- Disrupted routines due to GI symptoms
- Increased dependency on caregivers
- Limitations in dietary choices affecting nutrition
The interplay between GI disturbances and ASD symptoms necessitates a holistic approach to treatment, considering both physical and psychological well-being.
Effective management of GI symptoms can lead to improvements in overall health, potentially mitigating some behavioral symptoms and enhancing life experiences. Tailored interventions that address both the gut and the brain may unlock new pathways to support individuals with ASD in leading more comfortable and fulfilling lives.
The Link with Behavioral Symptoms
The intricate relationship between gastrointestinal (GI) issues and behavioral symptoms in autism spectrum disorder (ASD) is gaining recognition. Gut dysbiosis has been linked to ASD-like behaviors, including anxiety, stereotyped behavior, self-harm, and aggression. Addressing GI disturbances may offer a pathway to mitigating some autism symptoms.
Children with ASD often exhibit a range of comorbid conditions, such as learning difficulties and intellectual disabilities, which can manifest in various behavioral challenges. The presence of GI symptoms can exacerbate these issues, impacting daily life and overall well-being.
The severity of behavioral symptoms can vary widely among individuals with ASD, influenced by both neurological and gastrointestinal factors.
Understanding the connection between gut health and behavior is crucial for developing comprehensive treatment strategies. Interventions targeting gut health could lead to improvements in both GI and behavioral symptoms, offering hope for a more integrated approach to autism care.
The Microbiome's Role in Autism Spectrum Disorder
Gut Dysbiosis and Its Consequences
Gut dysbiosis represents a significant imbalance in the microbial ecosystem within the gastrointestinal tract. This condition is notably more prevalent in individuals with Autism Spectrum Disorder (ASD) than in the neurotypical population. The unique microbial signatures in ASD—characterized by reduced diversity and altered proportions of specific bacteria—may influence the disorder's neurological and behavioral manifestations.
The gut microbiota in ASD often shows a decrease in beneficial bacteria like Bifidobacterium and an increase in potentially pathogenic microbes. Such shifts can disrupt the delicate balance of the gut environment, leading to a cascade of effects on the host's health and well-being. The table below summarizes key differences in gut microbiota between ASD-diagnosed individuals and the control group:
| Bacteria | ASD Patients | Control Group |
|---|---|---|
| Bacteroidetes | Higher | Lower |
| Parabacteroides | Higher | Lower |
| Faecalibacterium | Lower | Higher |
| Bifidobacterium | Lower | Higher |
The interplay between various microbial kingdoms—bacteria, fungi, viruses—within the gut is intricate. Disruptions in this ecosystem can lead to a domino effect, impacting not just gastrointestinal health but also neurological function and behavior.
The consequences of gut dysbiosis extend beyond the gut itself, potentially affecting the central nervous system and contributing to the behavioral symptoms associated with ASD. Addressing these microbial imbalances may offer new avenues for therapeutic interventions, aiming to restore gut health and mitigate some of the challenges faced by those on the autism spectrum.
Microbial Diversity and Autism
The intricate ecosystem within our guts, teeming with trillions of microorganisms, is more than just a digestive aid; it's a pivotal player in our overall health. In the realm of autism spectrum disorder (ASD), research has unveiled a compelling link between the diversity of the gut microbiome and the condition itself.
Variations in microbial populations are not just incidental findings; they may influence the severity and manifestation of autism-related behaviors. A study highlighted a quasi-paired cohort strategy, revealing that certain microbes with detoxifying functions are often impaired in the guts of autistic children. This impairment could potentially contribute to the symptoms experienced by these individuals.
The balance of our gut flora is a delicate dance, with each microbe performing its own role. When this balance is disrupted, it can echo throughout the body, affecting everything from immune responses to neurological function.
Understanding the nuances of microbial diversity in autism is not just about cataloging bacteria; it's about piecing together a complex puzzle that may one day lead to more targeted and effective interventions. The following table summarizes key differences in gut microbiota between autistic individuals and their neurotypical counterparts:
| Microbial Group | Autistic Individuals | Neurotypical Individuals |
|---|---|---|
| Prevotella | Reduced incidence | Higher incidence |
| Detoxifying microbes | Impaired function | Normal function |
By delving into the microbial cosmos within us, we may find new pathways to enhance the quality of life for those on the autism spectrum. It's a frontier of discovery that holds promise for unraveling the mysteries of ASD and forging new inroads in treatment.
Metabolites and Their Effects on the Brain
The intricate dance between the gut and the brain is underscored by the presence of various metabolites that can influence neurodevelopment and behavior. Metabolites such as amino acids, lipids, and those involved in the urea cycle play a pivotal role in the gut-brain connection, particularly in the context of Autism Spectrum Disorder (ASD). These substances, often altered in the blood of autistic individuals, include tyrosine, tryptophan, and branched-chain amino acids (BCAAs), among others.
The metabolite profile in ASD reveals a complex interplay between mammalian and microbial pathways. For instance, the metabolism of tryptophan and BCAAs is closely linked to neurotransmitter pathways, which are essential for brain function and have been implicated in the pathogenesis of ASD. Elevated levels of certain bacterial metabolites, such as acetaminophen sulfate, have also been associated with autism-like behaviors.
Gut dysbiosis—an imbalance in the microbial community—can lead to increased intestinal permeability, allowing these metabolites to more easily cross the blood-brain barrier. This can affect the tight junction proteins that are crucial for maintaining the barrier's integrity. The result is a potential impact on the brain's development and function, manifesting in the behavioral symptoms characteristic of autism.
The metabolomics approach, sensitive to the interplay of genetic, microbial, dietary, and environmental factors, has shed light on the metabolic distinctions between autistic and neurotypical individuals.
Understanding these metabolic pathways is not just about deciphering the biochemical underpinnings of ASD; it's about unlocking new therapeutic avenues. By targeting specific metabolic dysfunctions, we may be able to alleviate some of the behavioral symptoms associated with autism, offering hope for more effective interventions.
Dietary Interventions and Autism
The Potential of Prebiotics and Probiotics
The gut microbiome's intricate role in Autism Spectrum Disorder (ASD) has turned the spotlight on dietary strategies that could influence neurodevelopment and behavior. Prebiotics and probiotics emerge as potential heroes in this narrative, offering a non-invasive way to modulate the gut environment. Prebiotics, found in foods like garlic, onions, bananas, and whole grains, act as fuel for beneficial gut bacteria, fostering a healthier gut microbiome.
Probiotics, on the other hand, introduce live beneficial bacteria directly into the gut. They are often found in fermented foods such as yogurt, kefir, and sauerkraut. The synergy between prebiotics and probiotics, known as synbiotics, could be particularly powerful in managing ASD symptoms. Here's a snapshot of how these dietary components can support gut health:
- Prebiotics: Stimulate growth of beneficial bacteria
- Probiotics: Introduce beneficial bacteria
- Synbiotics: Combine prebiotics and probiotics for enhanced effect
The potential of prebiotics and probiotics in managing ASD symptoms is not just theoretical. Research has shown promising results, with improvements in both gastrointestinal health and behavioral outcomes.
While the science is still evolving, the current evidence points to a significant role for dietary interventions in supporting individuals with ASD. It's a burgeoning field that holds promise for new therapeutic avenues, emphasizing the importance of gut health in overall well-being and neurological function.
Tailoring Nutrition for Gut Health
Customizing diet for individuals with autism involves a delicate balance of nutrients to support gut health and, by extension, cognitive and behavioral functions. A gluten-free diet, for instance, has been linked to positive changes in the gut microbiome (Polo et al., 2020). Similarly, protein digestion and the avoidance of microbial putrefaction are crucial (Sanctuary et al., 2018).
The gut-brain axis highlights the importance of dietary strategies that can influence neurodevelopment and behavior. While research is budding, the potential for dietary interventions to modulate the gut microbiome and alleviate ASD symptoms is promising.
The future of ASD management may well lie in the nuanced understanding of diet-microbiome interactions, offering new hope for those affected.
Here are some dietary considerations to optimize gut health:
- Increase fiber intake to promote beneficial bacteria growth
- Incorporate fermented foods rich in probiotics
- Limit processed foods and sugars that can disrupt microbial balance
- Ensure adequate hydration to maintain intestinal health
Each step towards a healthier gut is a step towards mitigating the challenges of ASD, echoing the sentiment that our well-being may be intertwined with the microscopic world within us.
Case Studies: Diet Modifications and Behavioral Changes
The interplay between diet and behavior in autism is a burgeoning field of study. Case studies reveal that dietary modifications can lead to significant behavioral changes in individuals with Autism Spectrum Disorder (ASD). Tailoring nutrition to address gut dysbiosis, a common issue in ASD, has shown promising results.
Personalized dietary approaches are key, considering individual sensitivities and preferences. The timing and duration of dietary interventions, along with their integration with other treatments, are critical for success. Regular monitoring ensures safety and efficacy.
The potential of dietary interventions to modulate brain function in ASD is substantial, warranting further research to optimize clinical practice.
Here's a snapshot of the impact of dietary interventions on behavioral outcomes:
- Improved social interaction: Some individuals exhibit more willingness to engage with others.
- Reduction in irritability: Dietary changes often correlate with decreased aggression and self-harm.
- Enhanced focus: A tailored diet can lead to better concentration and attention spans.
- Regulated sleep patterns: Adjustments in diet can help normalize sleep disturbances.
These outcomes underscore the importance of a holistic approach to treating ASD, where diet is a pivotal component.
Stool Testing as a Window into Gut Health
The Importance of Stool Analysis
Unlocking the secrets of the gut microbiome begins with a thorough stool analysis. Stool tests are the gateway to understanding the complex ecosystem within our gut, providing a detailed snapshot of the microbial landscape. These tests reveal not just the presence of pathogenic bacteria, but also the beneficial ones that are crucial for maintaining a healthy gut-brain connection.
Stool analysis is particularly transformative in the context of autism treatment. By pinpointing specific imbalances, healthcare providers can tailor interventions to the unique needs of each individual. This personalized approach is key to optimizing treatment outcomes and enhancing quality of life.
- Microbial Imbalances
- Digestive Function
- Targeted Interventions
Armed with insights from stool testing, interventions can be precisely directed to rebalance the gut, potentially alleviating some behavioral symptoms associated with autism.
Biomarkers for Gut Dysbiosis
Identifying biomarkers for gut dysbiosis is crucial in understanding and managing autism spectrum disorder (ASD). Biomarkers can signal an imbalance in the gut microbiota, which is often seen in individuals with ASD. These markers range from specific microbial species to metabolic byproducts that reflect the health of the gut ecosystem.
Gut dysbiosis in ASD is characterized by a less diverse microbiota, with significant differences in the presence of certain bacteria. For instance, levels of Bacteroidetes, Parabacteroides, and Faecalibacterium are altered, while beneficial bacteria like Coprococcus and Bifidobacterium are often found in decreased levels.
The identification of these biomarkers is not only diagnostic but can also guide targeted interventions to restore balance in the gut microbiome.
Here's a snapshot of key biomarkers associated with gut dysbiosis in ASD:
- Decreased levels: Coprococcus, Bifidobacterium
- Increased levels: Desulfovibrio, Caloramator
- Metabolic indicators: Mitochondrial dysfunction, abnormal gut microbiome metabolism
Understanding these biomarkers helps in the early intervention and personalized treatment of ASD, potentially improving the quality of life for affected individuals.
Interpreting Results for Personalized Treatment
The art of interpreting stool test results lies in the ability to tailor interventions to the unique gut microbiome of each individual with autism. Personalized treatment plans can be crafted by analyzing specific biomarkers indicative of gut dysbiosis. This approach not only addresses gastrointestinal symptoms but also holds promise for mitigating behavioral challenges associated with autism.
Stool analysis provides a non-invasive snapshot of the gut's health, revealing crucial information about microbial diversity and function. By understanding these results, clinicians can recommend dietary adjustments, probiotic supplements, or other therapies suited to the patient's specific needs.
The goal is to create a harmonious gut environment that supports overall well-being and neurological health.
Emerging research underscores the importance of individualized care. The Lancet Commission's recent report advocates for stepped care strategies that adapt over a person's lifetime, emphasizing the role of personalized treatment in effective autism care. As we move forward, the integration of stool test data into comprehensive care plans will become increasingly vital.
The Immune System's Role in the Gut-Brain Connection
Inflammation and Autism
The intricate dance between the immune system and brain development takes a unique turn in autism spectrum disorder (ASD). Inflammation is not just a response to injury; in ASD, it's a persistent state that can shape neurodevelopment. Studies have consistently shown elevated levels of pro-inflammatory cytokines in individuals with ASD, suggesting a chronic immune activation that may interfere with brain function.
Immune dysfunction in ASD is a complex affair, involving a cascade of interactions between various cell types and signaling molecules. For instance, cytokines such as IL-1\u03b2, IL-6, and IL-8 are often found at higher levels in the blood of autistic individuals, hinting at an ongoing inflammatory process. This imbalance not only affects gastrointestinal health but may also play a role in the behavioral symptoms associated with ASD.
The presence of certain cytokines can inhibit neurogenesis and promote neuronal death, while others may support brain growth and repair. The challenge lies in understanding how these molecules influence the brain's wiring and functioning in the context of autism.
The following table summarizes key cytokines and their observed levels in ASD:
| Cytokine | ASD Levels | Control Levels |
|---|---|---|
| IL-1\u03b2 | Elevated | Normal |
| IL-6 | Elevated | Normal |
| IL-8 | Elevated | Normal |
| IL-10 | Decreased | Normal |
By delving into the immune system's role, we can uncover new therapeutic avenues that target these inflammatory responses, potentially offering relief and improved outcomes for those on the autism spectrum.
The Enteric Nervous System and Immunity
The enteric nervous system (ENS) is often dubbed the 'second brain' due to its extensive network of neurons that govern the gastrointestinal tract. The ENS plays a pivotal role in the gut-brain connection, particularly in the context of autism, where immune dysregulation is frequently observed. The ENS not only manages digestion but also communicates with the brain, influencing emotional and cognitive functions.
Emerging evidence underscores the significance of the ENS in maintaining the integrity of barriers like the blood-brain barrier (BBB), which are crucial for protecting the brain from pathogens and toxins. This protective role is facilitated by the crosstalk between the microbiota and the immune system, which helps regulate the development of microglia and other immune cells within the central nervous system.
The bidirectional communication between the gut and the brain is mediated by a complex interplay of neuronal, immune, and endocrine signals.
Microbial residents in the gut can produce neurotransmitters and other bioactive compounds that affect the brain. Disruptions in this communication network may lead to neuroinflammation and behavioral changes associated with autism. Understanding the ENS's influence on immunity provides a foundation for exploring therapeutic avenues that target these intricate pathways.
Therapeutic Avenues Targeting Immune Responses
The quest for effective autism therapies has led to a focus on the immune system's role in the gut-brain connection. Innovative treatments aim to modulate immune responses, potentially alleviating autism symptoms. Marchezan et al. have categorized these interventions into two groups: those with direct anti-inflammatory or immunomodulatory effects, and those with secondary immunomodulatory capabilities observed during treatment.
- Direct interventions include radicicicol, celecoxib, and corticosteroids.
- Secondary interventions encompass risperidone, vitamin D, and omega-3.
These therapeutic strategies are not without challenges, as the complexity of the immune system and its interaction with the brain and gut in autism requires precise targeting to avoid unintended effects.
Emerging compounds like resveratrol and luteolin target specific pathways such as NF-κB and JAK/STAT, offering hope for more tailored treatments. The potential of these therapies lies in their ability to dampen neuroinflammation, a common thread in autism's diverse tapestry.
Emerging Research on the Gut Microbiome and Autism
Latest Findings and Studies
Emerging research in the gut microbiome's influence on autism spectrum disorder (ASD) is a rapidly evolving field. Recent studies highlight the promise of dietary interventions in potentially modulating brain function and behavioral symptoms in ASD. However, it's crucial to acknowledge that this research is still nascent, with much to be discovered about the intricate mechanisms involved.
The potential of dietary interventions in ASD is significant, yet it is accompanied by the need for personalized approaches and careful monitoring.
While the studies by Prehn-Kristensen and Wang et al. have opened new avenues, their findings require validation through larger cohorts to ensure reliability and applicability. The consensus among researchers is clear: the journey to fully understand the gut-brain connection in autism is just beginning, and the path ahead is filled with both challenges and opportunities.
- Further studies are necessary to establish evidence-based dietary recommendations.
- Personalized dietary approaches may be necessary for optimal outcomes.
- Integration with other evidence-based treatments is crucial.
- Safety considerations and regular monitoring are paramount.
Challenges in Gut Microbiome Research
The quest to unravel the gut microbiome's influence on autism is fraught with complexities. Selecting the right sequencing techniques and genome databases is pivotal, yet it's just the tip of the iceberg. Researchers must navigate a labyrinth of variables that shape the gut flora, such as dietary habits, GI dysfunction, and even geographical differences. These factors can significantly sway the microbial landscape during critical early childhood development stages, potentially impacting neurobehavioral outcomes.
The challenge is not only in capturing the vast diversity of the microbiome but also in interpreting the data in the context of autism's multifaceted nature.
Choosing an appropriate control group is another hurdle. The debate between using first-degree sibling non-affected (NT) controls versus unrelated NT controls is ongoing. Moreover, the intricacies of sampling procedures and bioinformatics analysis add layers of complexity. For instance, the 16S-rRNA gene sequencing, while informative about taxonomic composition, offers limited resolution and scant insight into microbial functions.
- Consideration of age, stress, and host genetics
- Documentation of dietary habits
- Impact of geographic location
- Influence of host physiology
These are just a few of the myriad factors that can confound the establishment of clear connections between gut microbiota and host neuroimmune homeostasis. As research progresses, the need for standardized methodologies and long-term safety studies becomes increasingly apparent, especially when considering interventions like fecal microbiota transplantation (FMT) therapies.
Future Directions for Understanding the Gut-Brain-Autism Triad
As we venture deeper into the enigmatic world of the gut-brain-autism triad, the horizon of research is expanding. The quest for clarity in the gut-brain connection as it relates to autism is paving the way for innovative approaches. With a focus on the gut microbiome, scientists are unraveling the intricate web of interactions that could unlock new therapeutic strategies.
- Understanding the genetic underpinnings that influence gut microbiota composition.
- Exploring the role of environmental factors in shaping the gut ecosystem.
- Investigating the impact of early-life nutrition on long-term neurological outcomes.
The potential of personalized medicine looms large, with stool testing and dietary interventions tailored to the individual's unique microbiome profile.
The integration of advanced computational methods and artificial intelligence is anticipated to enhance our ability to interpret complex data. This will facilitate a more nuanced understanding of the microbiome's influence on neurodevelopmental disorders. As research progresses, the translation of these findings into clinical practice could revolutionize the management of autism, offering hope for improved quality of life for individuals on the spectrum.
Behavioral Changes and Gut Microbiota
Correlation Between Gut Health and Behavioral Patterns
The intricate dance between gut health and behavior in autism is a focus of intense research. Gut dysbiosis, a state of microbial imbalance, has been linked to a range of behavioral symptoms in autistic individuals. These include anxiety, aggression, and repetitive behaviors, which can significantly impact daily life.
- Behavioral Improvements: Addressing gut health can lead to better mood regulation and reduced irritability.
- GI Symptoms and Behavior: GI issues correlate with behavioral manifestations like self-harm and stereotypy.
- Microbiome and Behavior: Studies show a connection between microbiota composition and stress responses.
While the exact mechanisms remain to be fully understood, the evidence points to a strong gut-behavior axis that could unlock new therapeutic avenues.
However, the causal relationships and temporal dynamics of these changes are complex and multifaceted, involving factors such as diet, GI comorbidities, and individual differences. This complexity underscores the need for personalized approaches in addressing gut health to improve behavioral outcomes in autism.
Interventions Aimed at Modifying the Microbiome
Harnessing the power of the gut microbiome, interventions are being tailored to address the unique needs of individuals with autism. Probiotic treatments stand at the forefront, introducing beneficial bacteria to foster a balanced microbial community. These interventions are not just about adding good bacteria; they're about reshaping the entire ecosystem within the gut.
Prebiotics also play a crucial role, serving as the fuel that feeds the beneficial bacteria. Incorporating foods like garlic, onions, bananas, and whole grains into the diet can selectively stimulate the growth of health-promoting microbes. This dietary strategy is a beacon of hope for managing ASD symptoms through gut health.
Antimicrobial strategies target the unwanted guests: pathogenic microorganisms. By using specific agents or herbal supplements, these interventions aim to purge the pathogens and pave the way for a healthier gut microbiota.
The goal is clear: modulate the gut microbiota to improve behavioral outcomes and quality of life for those on the autism spectrum.
Here's a snapshot of the interventions:
- Probiotic Treatments: Introducing beneficial bacteria to balance the gut microbiome.
- Prebiotic-Rich Diet: Stimulating the growth of good bacteria with specific foods.
- Antimicrobial Strategies: Eliminating pathogenic microorganisms to restore gut health.
Assessing Outcomes and Efficacy
When evaluating the success of interventions targeting the gut microbiota in autism, it's essential to consider both the scientific rigor and the real-world impact. Outcomes must be measurable, meaningful, and sustainable to truly assess efficacy.
Evidence quality is paramount, and tools like the Critical Appraisal Skills Program (CASP) checklist help ensure the transparency and reliability of research findings. A robust level of evidence score, established through consensus methods, supports the validity of study results.
- Safety and regular monitoring
- Integration with other evidence-based treatments
- Impact on core ASD symptoms and quality of life
The ultimate goal is to implement dietary and microbial interventions that are both safe and effective, enhancing the lives of individuals with autism.
It's not just about the numbers; it's about the nuanced changes in behavior and well-being that can transform daily experiences for autistic individuals and their families.
Clinical Perspectives on Treating Autism Through the Gut
Case Studies from Pediatric Nutritionists
Pediatric nutritionists play a pivotal role in understanding how dietary interventions can support children with autism. Case studies reveal the transformative impact of tailored nutrition plans. For instance, a study by Knivsberg et al. (1995) followed the effects of a gluten-free and casein-free diet on autistic behaviors, showing significant improvements in some children.
Autism Spectrum Disorder (ASD) is complex, and no one-size-fits-all diet exists. However, nutritionists have documented cases where specific dietary changes correlate with behavioral enhancements. These include the reduction of processed foods, introduction of omega-3 fatty acids, and ensuring adequate vitamin and mineral intake.
The careful monitoring of dietary adjustments can lead to notable changes in communication, social interactions, and overall well-being.
A summary of key interventions and outcomes is presented below:
- Elimination of certain allergens and irritants (e.g., gluten, casein)
- Incorporation of nutrient-dense foods
- Supplementation with vitamins and minerals
- Regular assessment and adjustment of dietary plans
These interventions, while not a cure, offer a complementary approach to traditional therapies. They underscore the importance of a holistic perspective in treating ASD, considering the gut-brain connection and its influence on behavior.
Integrative Approaches to Therapy
Integrative therapy in autism combines various modalities to address the complex needs of individuals on the spectrum. Personalization is key, as each person may respond differently to interventions. An integrative approach often includes a mix of behavioral therapies, educational interventions, and family involvement.
Play therapy, music therapy, and family-centered interventions are pillars of this holistic strategy. They aim to improve communication, social skills, and emotional regulation, while also supporting the family unit.
- Behavioral Therapies: Applied Behavior Analysis (ABA), Cognitive Behavioral Therapy (CBT)
- Educational Interventions: Specialized curriculums, Individualized Education Programs (IEPs)
- Family Involvement: Parent training, Sibling support groups
Embracing the uniqueness of each autistic individual, integrative therapy tailors treatment plans to foster maximum potential.
By considering the individual's strengths and challenges, therapists can craft a comprehensive plan that may include novel and traditional therapies alike. The goal is to create a supportive environment that encourages growth and learning.
Patient and Caregiver Education
Empowering patients and caregivers with the knowledge to manage autism through the gut is a cornerstone of effective treatment. Education is not just about imparting knowledge; it's about fostering independence and confidence. Tailored educational programs can guide families through the complexities of dietary interventions and the importance of integrating them with other evidence-based treatments.
- Safety considerations and regular monitoring are paramount to ensure that dietary changes are both safe and beneficial.* Here's a quick guide to recommended behavioral and educational interventions:
- ABA (Applied Behavior Analysis)
- TEACCH (Treatment and Education of Autistic and related Communication-handicapped Children)
- ESDM (Early Start Denver Model)
- PRT (Pivotal Response Treatment)
- PACT (Parent-mediated Communication-focused Treatment)
- RIT (Reciprocal Imitation Training)
- JA (Joint Attention)
It's essential to remember that every individual with autism is unique, and what works for one may not work for another. Personalization of treatment plans is key.
Conclusion
The exploration of the gut-brain connection in Autism Spectrum Disorder (ASD) has unveiled a fascinating and intricate link that holds promise for innovative interventions. The evidence presented underscores the prevalence of gastrointestinal issues in individuals with autism and the significant role of the gut microbiome in influencing neurological health and behavior. While the exact mechanisms remain to be fully elucidated, the potential of dietary modifications and targeted therapies to alleviate symptoms and improve quality of life is evident. As research continues to advance our understanding of the gut-brain axis, it is becoming increasingly clear that nurturing a healthy gut microbiome could be a key component in managing ASD. The future of autism therapy may well lie in the delicate balance of our internal ecosystems, emphasizing the importance of integrated approaches that consider the whole body in the quest for well-being.
Frequently Asked Questions
What is the gut-brain axis and how does it relate to autism?
The gut-brain axis is a bidirectional communication system linking the gastrointestinal tract with the central nervous system. In autism, disruptions in this axis can manifest as gastrointestinal issues and influence neurodevelopment and behavior.
How common are gastrointestinal issues in individuals with autism?
Gastrointestinal issues are remarkably common in individuals with autism, with many experiencing conditions such as constipation, diarrhea, and irritable bowel syndrome (IBS).
Can dietary interventions impact behavioral symptoms in autism?
Yes, dietary interventions, especially those involving prebiotics and probiotics, can modify the gut microbiome and have shown potential in influencing behavioral outcomes in individuals with autism.
What is gut dysbiosis and how does it affect individuals with autism?
Gut dysbiosis refers to an imbalance in the gut microbiome's composition and diversity. In autism, it can lead to inflammation, compromised immune function, and production of metabolites that may affect the central nervous system.
Why is stool testing important in the context of autism?
Stool testing can provide insights into gut health by identifying issues like gut dysbiosis. It can inform personalized treatment approaches for individuals with autism by highlighting specific imbalances in the gut microbiome.
How does the immune system interact with the gut-brain connection in autism?
The immune system can contribute to inflammation and interact with the enteric nervous system, affecting the gut-brain axis. This interaction may play a role in the neurodevelopmental aspects of autism.
What are the latest research findings on the gut microbiome's role in autism?
Recent studies suggest that alterations in the gut microbiome may contribute to autism by affecting gut-brain axis connectivity, neurodevelopment, and behavior. The precise mechanisms are still being explored.
Are there any correlations between changes in gut microbiota and behavioral patterns in autism?
Yes, emerging research indicates a correlation between gut microbiota and behavioral patterns in autism. Interventions aimed at modifying the microbiome may lead to behavioral changes and improved outcomes.
On This Page
Frequently asked questions
How does the autism gut-brain connection influence behavior and gastrointestinal health?
What are common autism gastrointestinal issues, and how can they affect daily life?
How can sensory-friendly autism support help manage gut-related discomfort?
What role do autism dietary interventions like prebiotics and probiotics play in improving gut health?
Are there autism-friendly products, such as calming blankets or sensory tools, that support gut-brain wellness?
How can stool testing guide personalized treatment for gut microbiome autism imbalances?
What is the relationship between gut dysbiosis and behavioral symptoms in autism?
How does the immune system interact with the gut-brain axis in autism spectrum disorder?
Can Autism-themed decor or comfortable clothing like t-shirts contribute to a calming environment that supports gut and brain health?

About the HeyASD.com Team
Autistic‑owned • Values‑led • Sensory‑friendly design
We are autistic creators, writers, and advocates dedicated to producing resources that are practical, sensory-aware, and grounded in lived experience. Our mission is to make information and products that support the autistic community accessible to everyone, without jargon or condescension. Learn more about our team.
This article is written from lived autistic experience and an evidence-aware perspective. It is for general informational purposes only and should not be taken as medical, legal or therapeutic advice.
Always consult a qualified clinician or occupational therapist for individual needs and circumstances.

About Our ASD Blog
HeyASD is more than a store, it’s a calm, supportive space for autistic adults and the people who care about them. Explore identity-affirming stories, sensory regulation tools, and uplifting resources from our community.
Thank you for reading. We hope these resources bring comfort and clarity.