Probiotics and Gut Health in Autism

Written by HeyASD.com Team
The intricate relationship between the gut microbiome and neurological health has become a key area of focus, especially in understanding autism spectrum disorders (ASD). Emerging evidence suggests that the diverse ecosystem of bacteria within our gut, known as the gut microbiome, has significant implications for the development and management of ASD. This article delves into the gut-brain connection, the influence of gut microbiota on autism, the potential of probiotics as a therapeutic approach, and the use of stool testing to gain insights into gut health in individuals with autism. Moreover, it explores dietary interventions, fecal microbiota transplantation, the immune system's role, and the latest research in the field, all aimed at improving the quality of life for those affected by autism.
Key Takeaways
- Alterations in the gut microbiome composition are linked to autism, potentially affecting immune function and the central nervous system.
- Stool testing can reveal microbial imbalances and help assess the effectiveness of dietary and probiotic interventions in ASD.
- Probiotic supplementation has shown promise in alleviating gastrointestinal symptoms and may correlate with reductions in autism severity.
- Dietary changes, such as gluten-free and casein-free diets, can improve gut health and behavioral symptoms in some individuals with autism.
- Fecal microbiota transplantation and its long-term effects on autism symptoms represent an emerging area of research with promising preliminary results.
Exploring the Gut-Brain Connection in Autism
Understanding the Gut-Brain Axis
The gut-brain axis represents a complex communication network that intricately connects our digestive system with our brain. Disruptions in this axis can manifest as gastrointestinal issues, which are notably prevalent among children with autism. These issues range from constipation to irritable bowel syndrome (IBS), adding to the challenges faced by these individuals.
The microbiota-gut-brain axis (MGBA) is pivotal in maintaining this communication. It involves a symphony of signals that the brain interprets to regulate both mental and physical functions. The gut microbiota, often considered an 'essential organ,' influences brain neurophysiology and behavior through various signaling pathways, including neuronal, immune, and endocrine mechanisms.
Bacteria within the gut produce neurotransmitters that are crucial for modulating neuronal activity within the axis. These neurotransmitters serve as signaling molecules between host and microbe, highlighting the significance of the gut's neuro-hormonal functions.
Understanding the gut-brain axis in autism is vital for developing targeted interventions. By addressing the microbial imbalances, we can potentially alleviate some of the GI symptoms and improve the overall well-being of those on the autism spectrum.
Neurological Impact of Gut Microbiota
The intricate web of communication between our gut microbiota and the brain is a frontier in understanding autism's complexities. The gut microbiota contributes to the maintenance of human health, including the central nervous system, by engaging in a dynamic dialogue that influences neurological function. This dialogue is particularly relevant in autism, where altered gut microbial communities are often observed.
Neurotransmitters of both the peripheral and central nervous systems are key players in this interaction. Gut bacteria can synthesize and metabolize these chemical messengers, acting as crucial links in the gut-brain axis. The resulting host-microbe signaling has profound implications for neurobehavioral development and may influence the trajectory of neurodevelopmental disorders.
The study of microbial dynamics in neurodevelopmental disorders is complex, influenced by a myriad of factors such as age, diet, and genetics.
Understanding these interactions is vital, as they may unlock new therapeutic strategies targeting the microbiota to alleviate symptoms associated with autism. The potential for microbiota-targeted interventions to improve symptoms opens a promising avenue for research and treatment.
The Role of the Vagus Nerve
The vagus nerve stands as a pivotal channel in the gut-brain axis, orchestrating a symphony of signals that influence our well-being. In autism, the vagus nerve's function is particularly intriguing, as it may hold keys to understanding certain behaviors, such as visual stimming. This nerve is a highway for neurotransmitters that modulate neuronal activity, linking the gut's microbiota to the brain's neurophysiology.
Disruptions in the vagus nerve can lead to a cascade of gastrointestinal and neurological issues. These disruptions are often observed in children with autism, manifesting as common GI problems that exacerbate distress and may affect neurobehavioral development.
The gut microbiota, through the vagus nerve, contributes to the maintenance of human health, impacting organs including the CNS.
Understanding the vagus nerve's role could unlock new therapeutic strategies, potentially easing the burden of autism's gastrointestinal and neurological manifestations.
The Gut Microbiome's Influence on Autism Spectrum Disorders
Diversity and Composition of Gut Microbiota in Autism
The gut microbiota's diversity and composition are pivotal in understanding Autism Spectrum Disorders (ASD). Studies reveal significant differences in the intestinal microbiota of children with ASD compared to their neurotypical peers. These differences may influence neurological development and behavior.
Prevotella, a bacterium associated with the fermentation of carbohydrates and fiber, is notably reduced in autistic children. This reduction could affect the production of short-chain fatty acids (SCFAs), which are crucial for gut health and neurodevelopment.
The composition of gut microbiota in ASD is not just about the presence or absence of specific microbes; it's about the balance and function they bring to the host.
The table below summarizes key findings from recent studies on gut microbiota in ASD:
| Study Reference | Key Finding |
|---|---|
| Liu et al., 2019 | Altered microbiota composition and function |
| Wang et al., 2012 | Elevated fecal SCFA and ammonia concentrations |
| Iglesias-Vázquez et al., 2020 | Systematic differences in microbiota composition |
| Kang et al., 2013 | Reduced incidence of Prevotella and other fermenters |
Understanding these microbial imbalances opens the door to targeted interventions, such as probiotic supplementation, to restore a healthy gut ecosystem and potentially alleviate some ASD symptoms.
Inflammation and Immune Function
The gut microbiome's intricate role extends beyond digestion, significantly influencing the immune system. An imbalance in gut microbiota can lead to altered immune responses, potentially exacerbating inflammation. This is particularly relevant in Autism Spectrum Disorders (ASD), where such imbalances may contribute to both gastrointestinal and neurological symptoms.
Inflammation and immune dysregulation are often observed in individuals with ASD. For instance, variations in microbial populations—like increased Clostridales and decreased Dorea, Blautia, and Sutterella—have been linked to changes in pro-inflammatory cytokines. These cytokines, including IL-1\u03b2, IL-6, IL-8, and IL-12p40, can impact the brain by traveling through the bloodstream.
The relationship between gut microbiota and immune function is a key factor in understanding ASD. Disruptions in this relationship may manifest as heightened inflammatory markers and altered cytokine profiles, which are associated with ASD severity.
The following list highlights the cytokines frequently found at elevated levels in individuals with ASD, indicating immune system dysregulation:
- IL-1\u03b2
- IL-6
- IL-8
- IL-12p40
These findings underscore the potential of targeting gut microbiota to modulate immune function and inflammation in ASD, offering a promising avenue for therapeutic intervention.
Metabolites and Their Effects on the CNS
The intricate dance between gut microbes and the central nervous system (CNS) is choreographed by a diverse cast of metabolites. These biochemical emissaries, including neurotransmitters and short-chain fatty acids (SCFAs), are pivotal in modulating brain function. Bacteria in the gut synthesize and metabolize neurotransmitters, which serve as critical signaling molecules within the gut-brain axis.
Metabiotics such as amino acids and vitamins possess properties that extend beyond digestion, influencing the immune and nervous systems.
The impact of these metabolites on neurobehavioral trajectories is profound, especially in the context of Autism Spectrum Disorders (ASD). Monitoring changes in metabolites can reveal insights into symptomatology and behavioral shifts. For instance, probiotics can alter the body's acidic environment, inhibiting harmful bacteria and promoting a balanced microbiota.
- Neurotransmitters: Modulate neuronal activity
- SCFAs: Affect the immune and nervous systems
- Vitamins: Contribute to neuro-hormonal functions
Understanding these interactions is crucial for developing targeted interventions that may alleviate some of the challenges associated with ASD.
Probiotics as a Therapeutic Strategy for Autism
Efficacy of Probiotic Supplementation
The quest to alleviate the challenges of autism spectrum disorders (ASD) has led to the exploration of probiotics as a potential ally. Probiotic supplementation has shown promise in improving gastrointestinal (GI) symptoms, which are often prevalent in individuals with ASD. Studies indicate a significant reduction in constipation scores, stool consistency, and abdominal pain, suggesting a direct benefit to gut health.
Probiotics may also play a role in the eradication of certain infections, such as Helicobacter pylori, known to cause chronic inflammation. While results are encouraging, the scientific community urges caution due to heterogeneity in trial outcomes. The effectiveness hinges on specific strains, dosages, and treatment durations, underlining the need for further research.
The interplay between probiotics and gut microbiota in ASD is complex, yet the potential for symptom relief is an avenue worth pursuing.
Here's a snapshot of the impact of probiotics on GI symptoms in ASD:
- Significant reduction in constipation scores
- Improvement in stool consistency
- Decrease in flatulence
- Alleviation of abdominal pain
These findings underscore the importance of a tailored approach to probiotic therapy, considering the unique microbial landscape of each individual with ASD.
Improvements in Gastrointestinal Symptoms
The link between probiotics and gastrointestinal (GI) symptom relief in Autism Spectrum Disorder (ASD) patients is gaining empirical support. Studies reveal a significant reduction in GI disturbances following probiotic and Fecal Microbiota Transplantation (FMT) interventions. Notably, a substantial decrease in symptoms such as constipation, stool inconsistency, and abdominal pain has been documented.
Probiotic supplementation has been correlated with both an increase in beneficial gut bacteria, like Bifidobacteria, and a decrease in constipation severity. This dual effect underscores the potential of probiotics as a multi-faceted therapeutic approach for ASD-related GI issues.
The persistence of symptom improvement post-treatment suggests a lasting impact on gut health, which could translate into long-term benefits for ASD individuals.
The following table summarizes key findings from recent studies:
| Study | Improvement in GI Symptoms | Correlation with Autism Severity |
|---|---|---|
| Kang et al. (2017) | 89% of subjects showed improvement | Persistent up to 8 weeks post-FMT |
| Shaaban et al. (2018) | Significant reduction in constipation, flatulence, and pain | Strong correlation (r = 0.674, p = 0.0001) with autism severity reduction |
These findings not only highlight the therapeutic potential of probiotics but also suggest a promising avenue for reducing autism severity through gut health management.
Correlation with Autism Severity Reduction
The quest to alleviate the challenges of autism has led to a keen interest in the gut microbiome's role in influencing ASD severity. Probiotic supplementation has emerged as a promising avenue, with studies hinting at a potential correlation between gut health and autism severity reduction.
One study by Ahmed et al. (2020) compared intestinal microbiota in individuals with mild to moderate ASD against those with severe ASD. The results revealed a higher presence of Firmicutes taxa in severe cases. This aligns with earlier research by Tomova et al. (2015), which reported a lower Bacteroidetes to Firmicutes ratio in children with more pronounced ASD symptoms.
While the data is still being pieced together, these findings suggest that modulating the gut microbiota through probiotics could influence the severity of ASD symptoms.
The implications of these findings are profound, as they open up new avenues for therapeutic interventions. By targeting the gut microbiome, there is potential not just for symptom management but for a tangible reduction in autism severity. This could lead to improved quality of life for individuals on the spectrum and their families.
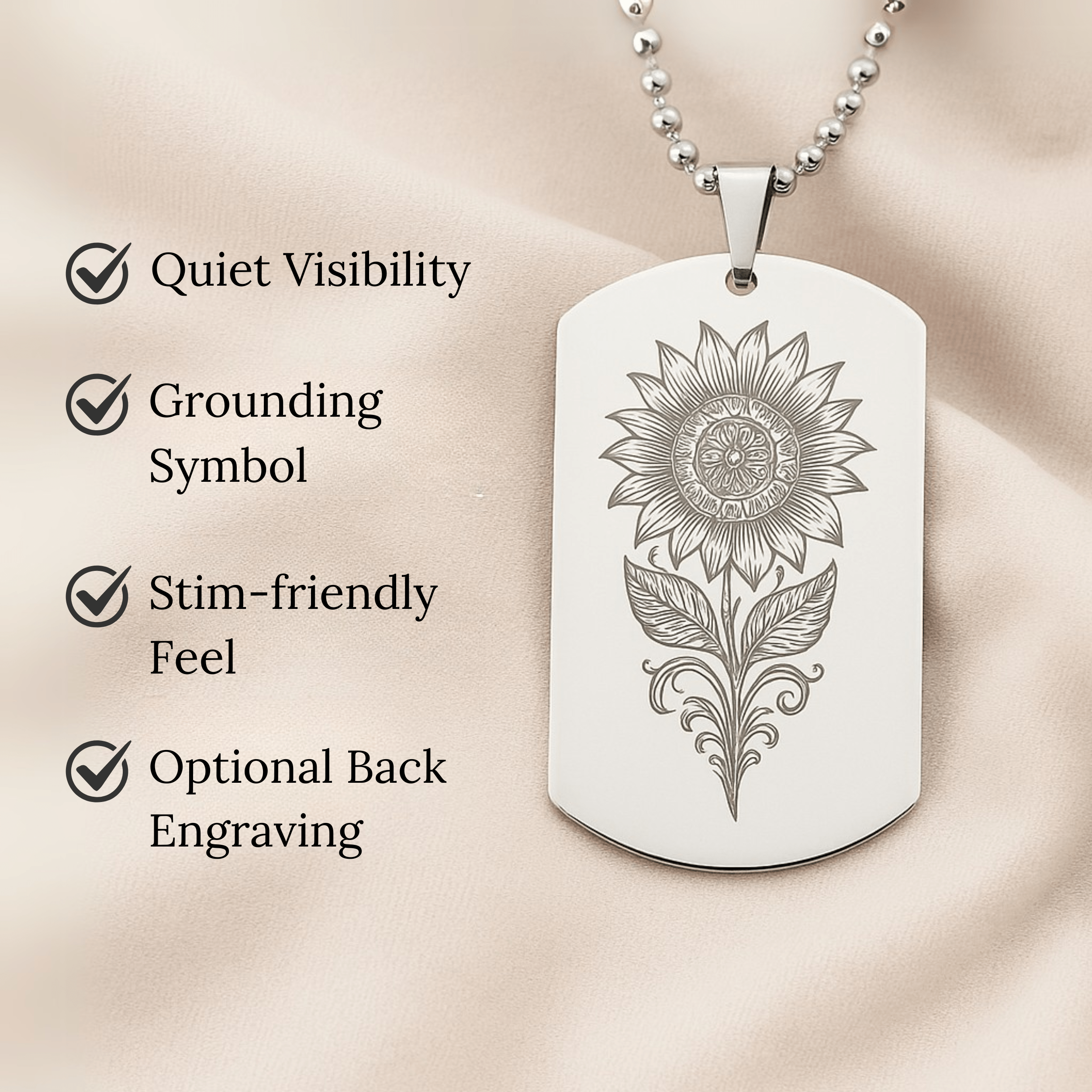
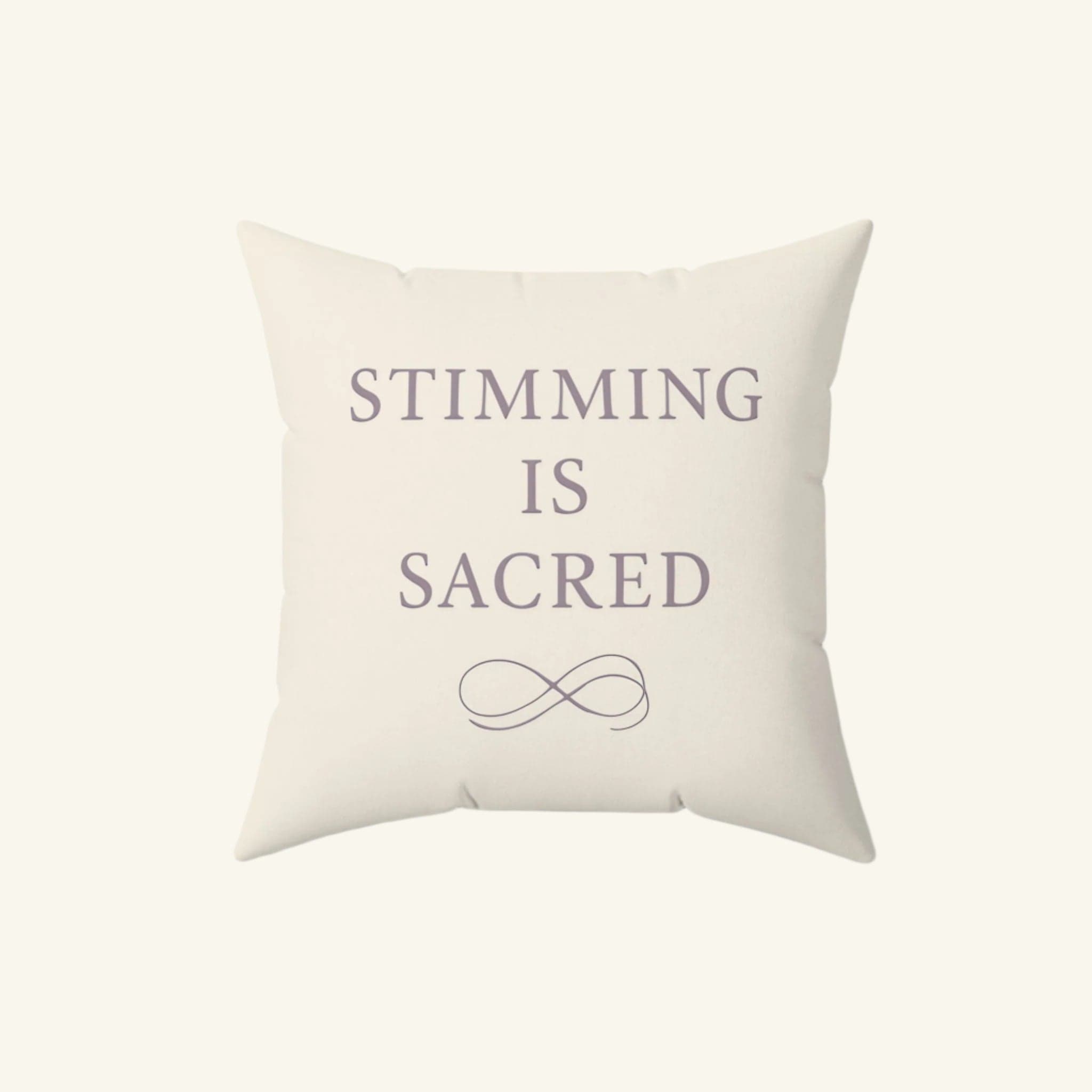
For those looking to celebrate their journey and promote autism awareness, the autism store offers a range of autism-themed wall art, apparel, and decor. It's a place where creativity meets advocacy, with free shipping on orders over $49.
Stool Testing: A Window into Gut Health in Autism
Identifying Microbial Imbalances
Stool tests such as the GI Map are pivotal in pinpointing microbial imbalances in the gut, a condition known as dysbiosis. Dysbiosis can lead to a cascade of issues, including inflammation, impaired digestion, and compromised nutrient absorption. By identifying specific bacteria, both beneficial and pathogenic, clinicians can tailor interventions with probiotics, prebiotics, and antimicrobial strategies.
The intricate interplay between our gut microbiota and overall health is undeniable. In autism, where gut health may influence neurological outcomes, understanding these microbial communities becomes even more crucial. Factors such as diet, stress, and genetics all contribute to the composition of gut microbiota, making the task of identifying imbalances a complex but necessary endeavor.
The goal is to restore a balanced microbial ecosystem, which may in turn support better health outcomes in individuals with autism.
Here's a snapshot of what stool tests examine:
- Abundance and diversity of bacteria
- Presence of pathogenic microorganisms
- Levels of inflammation-inducing agents
- Enzymatic activity and vitamin production by microbes
- Acidic environment alterations and its effects
By assessing these parameters, researchers and clinicians can gain insights into the gut-brain connection and its implications for autism spectrum disorders.
Assessing the Effectiveness of Dietary Interventions
To gauge the success of dietary interventions in individuals with autism, a multifaceted approach is essential. Tracking changes in gastrointestinal symptoms is a primary indicator of intervention efficacy. However, the impact on overall well-being and behavior also provides critical insights.
Stool testing emerges as a key tool in this assessment, offering a glimpse into the gut microbiome's response to dietary changes. The following table summarizes findings from recent studies:
| Study Reference | Participant Group | Intervention | Key Outcomes |
|---|---|---|---|
| Dror et al. (2017) | Mixed ages | Synbiotic supplementation | Improved anthropometry, lipid profile |
| Tonucci et al. (2017) | Adults with type 2 diabetes | Probiotics | Positive impact on nutritional status |
Consistent monitoring over time allows for the identification of patterns and the fine-tuning of dietary strategies to optimize gut health.
The interplay between diet and the gut microbiome is complex, and individual responses can vary widely. Therefore, personalized dietary plans, informed by stool test results and clinical observations, are paramount in achieving the best outcomes for those on the autism spectrum.
Monitoring Probiotic Treatment Outcomes
Monitoring the outcomes of probiotic treatments in individuals with autism is crucial for understanding their efficacy and tailoring interventions. Regular assessment of gastrointestinal symptoms and behavioral changes is a cornerstone of this process. Through metabolomic analysis of biological samples such as plasma, urine, and feces, clinicians can observe the direct impact of probiotics on the gut microbiome and overall health.
The goal is to restore a balanced microbiota, which in turn may alleviate clinical symptoms and improve quality of life.
Studies have shown varied results, with some indicating significant improvements in gut microbiota profiles and a reduction in gastrointestinal (GI) symptoms. For instance, a mix of Lactobacillus and Bifidobacteria strains administered to individuals with autism led to observable changes in their gut microbiota and symptomatology. To illustrate these findings, consider the following table summarizing outcomes from different studies:
| Study Type | Probiotic Strains | Outcome | Reference |
|---|---|---|---|
| Randomized Clinical Trial | Lactobacillus | 100% H. pylori eradication rate | [123] |
| Open Label Single Center | L. reuteri | Reduction in urease activity | [92] |
| Randomized Clinical Trial | Bifidobacterium, Lactobacillus | Improved eradication success rate | [124] |
It's important to note that while some studies report positive outcomes, others caution against heterogeneity among trials, suggesting that individual responses to probiotic treatments can vary significantly. Therefore, ongoing monitoring and research are essential to fully understand the potential of probiotics in managing autism-related gut health issues.
Dietary Interventions and Their Impact on Gut Health
Gluten-Free and Casein-Free Diets
The quest for optimal gut health in individuals with autism often leads to dietary experimentation, with the Gluten-Free Casein-Free (GFCF) diet being a notable example. Parents and caregivers have observed behavioral and communicative enhancements after eliminating gluten and casein, proteins found in wheat and dairy products, respectively. However, the scientific community remains cautious, as evidence for the GFCF diet's universal efficacy is still emerging and varies from person to person.
While some studies suggest a connection between dietary changes and improvements in gastrointestinal (GI) symptoms, the results are not uniform across the autism spectrum. The table below summarizes the potential outcomes of a GFCF diet based on observational studies:
| Outcome | Frequency of Improvement Reported |
|---|---|
| Behavior | Often |
| Communication | Sometimes |
| GI Symptoms | Frequently |
It's important to note that dietary interventions should be personalized and closely monitored to ensure nutritional adequacy and to assess their impact on the individual's well-being.
In the context of autism and gut health, the Bacteroides ratio and bifidobacterial numbers have shown changes with dietary adjustments. This highlights the intricate relationship between diet, the microbiome, and autism symptoms. As research progresses, the integration of probiotics, omega-3 fatty acids, and other supplements may complement dietary strategies to address deficits and support overall health.
Nutritional Status and Gut Microbiome
The intricate dance between nutritional intake and the gut microbiome plays a pivotal role in the overall health of individuals with autism. A balanced diet is crucial for maintaining a diverse and robust gut microbiota, which in turn can influence neurological development and function.
Gut microbial communities are significantly shaped by dietary patterns, particularly in early life. For those on the autism spectrum, dietary restrictions or preferences can lead to a less varied gut microbiome, potentially impacting cognitive and behavioral outcomes.
- Dietary Patterns: Often characterized by selectivity and rigidity.
- Gut Microbiota Diversity: Can be reduced due to limited dietary variety.
- Neurodevelopmental Impact: Potential influence on brain function and behavior.
The interplay between diet and gut health is a critical area of focus for improving the quality of life for individuals with autism.
Understanding the relationship between nutritional status and gut microbiome composition is essential for developing targeted interventions. By optimizing diet, we may be able to support a healthier gut microbiome, which could translate into positive neurological and behavioral effects.
Case Studies and Observational Findings
The landscape of autism research is ever-evolving, with case studies and observational findings providing valuable insights into the gut-brain connection. Diversity in gut microbiota has been a focal point, with studies revealing both commonalities and discrepancies among individuals with autism.
In particular, a reduction in the genus Prevotella has been noted across multiple studies, suggesting a potential biomarker for ASD. However, the variability in results underscores the complexity of the microbiome and its relationship with autism. The sample sizes, often small, may contribute to these inconsistencies, highlighting the need for larger, more robust studies.
- Conflicting results in microbial sequencing
- Geographical diversity in study populations
- Variations in bioinformatics analyses
The interplay between gut health and autism is intricate, with each study adding a piece of the puzzle to our understanding.
Further research is essential to unravel the nuances of this relationship, with the ultimate goal of enhancing therapeutic strategies for individuals on the autism spectrum.
Fecal Microbiota Transplantation (FMT) in Autism
Clinical Trials and Outcomes
The quest for effective interventions in autism has led to a surge in clinical trials exploring the potential of fecal microbiota transplantation (FMT). Systematic reviews and registrations, such as those found on clinicaltrials.gov, provide a framework for assessing the quality and outcomes of these trials. However, the diversity of probiotic strains and formulations used across studies makes direct comparisons challenging.
A rigorous approach to study selection and quality assessment is crucial. Methods include searching databases like PubMed and Cochrane for relevant keywords and conducting secondary reviews of references. This meticulous process ensures that only the most pertinent studies are considered, paving the way for reliable conclusions.
The need for medical recommendation before choosing specific probiotic products is underscored by the variability in trial outcomes.
Future research must prioritize high-quality studies and advanced monitoring to bridge the gaps in our understanding. The involvement of regulatory agencies is also essential to guide patients and practitioners in making informed decisions about probiotic use in autism.
Behavioral and Inflammatory Responses
The intricate dance between the gut microbiome and the immune system can manifest in both behavioral changes and inflammatory responses in individuals with autism. Elevated levels of pro-inflammatory cytokines, such as IL-1\u03b2, IL-6, IL-8, and IL-12p40, have been linked to more pronounced autism symptoms. These cytokines, acting as messengers of the immune system, can influence behavior by altering neurological function.
The gut microbiome's metabolites and molecular components are pivotal in signaling the immune system, which in turn affects both gut health and neurological outcomes.
A study by Cao et al found a positive correlation between plasma IL-6 levels and the severity of autism symptoms, suggesting that the immune response is intimately connected with behavioral manifestations. This connection is further supported by the presence of specific microbial taxa, such as Desulfovibrio, which are associated with increased ASD severity.
| Cytokine | Change in Levels | Associated Behavior |
|---|---|---|
| IL-1\u03b2 | Elevated | More abnormal behavior |
| IL-6 | Elevated | Increased ASD severity |
| IL-8 | Elevated | - |
| IL-12p40 | Elevated | - |
Understanding these relationships opens the door to potential therapeutic interventions targeting the gut microbiome to modulate immune responses and improve behavioral outcomes in autism.
Long-term Effects and Safety Considerations
When considering fecal microbiota transplantation (FMT) for autism, long-term effects and safety are paramount. Careful monitoring is essential, especially for vulnerable groups such as immunosuppressed individuals and those with severe underlying diseases. Adverse effects, though not commonly reported, can be significant and include the risk of probiotics translocating across the gut wall.
FMT's clinical benefits are promising, yet the field is riddled with knowledge gaps. The heterogeneity of studies and the variety of probiotic strains used make it challenging to draw definitive conclusions. Moreover, the lack of transparency in production processes complicates product comparison and informed decision-making.
It is imperative to only undertake FMT under medical supervision, with a clear understanding of the potential risks and benefits. Future research must aim to standardize methodologies and enhance monitoring to ensure patient safety.
The following points highlight key safety considerations:
- Consultation with healthcare professionals before starting FMT.
- Recognition of increased risk in specific patient groups.
- The necessity for advanced monitoring mechanisms.
- Urgent need for high-quality, standardized research.
The Immune System's Role in Autism and Gut Health
Autoimmunity and Gastrointestinal Dysfunction
The prevalence of functional gastrointestinal disorders (FGID), now known as disorders of gut-brain interaction (DGBI), is notably high among individuals with Autism Spectrum Disorder (ASD). These conditions can severely disrupt the bidirectional communication within the microbiota-gut-brain axis (MGBA), leading to a cascade of health issues.
Autoimmunity arises when the immune system mistakenly attacks the body's own cells, a phenomenon that can be triggered by pathogens with molecular mimicry. Such pathogens can cause cross-reactions that may lead to neuroinflammation and behavioral disorders. In ASD, this is particularly concerning as the immune response can exacerbate gastrointestinal symptoms and potentially influence neurological outcomes.
Gastrointestinal dysfunction in autism is not just a peripheral issue; it is intricately linked with the central nervous system. The following points highlight the complex interplay:
- Molecular mimicry by pathogens can lead to immunological cross-reactions.
- These reactions contribute to neuroinflammation and behavioral affective disorders.
- Gastrointestinal symptoms in ASD can be indicative of broader immune dysregulation.
The gut-brain-immune nexus in autism demands a nuanced approach to treatment, considering both the neurological and gastrointestinal dimensions of the disorder.
Probiotics and Immune Modulation
The interplay between probiotics and the immune system is a cornerstone of gut health, particularly in the context of autism. Probiotics have been shown to alter the intestinal microbiota, enhancing the body's immune response. By modulating both humoral and cellular immune responses, these beneficial bacteria strengthen the immune defenses, potentially impacting the severity of autism-related symptoms.
Probiotics and prebiotics not only influence cellular metabolism and proliferation but also fortify epithelial barrier functions. This is crucial for maintaining gut integrity and preventing unwanted substances from entering the bloodstream. Early colonization by Bacteroides and bifidobacterium species is vital for developing immunological control, as the gut microbiome is a dynamic entity shaped by various factors, including a mother's diet.
Probiotics assist in metabolizing food to improve nutrient absorption and digestion, boost mucosal immunity, lower gut inflammation, and promote neurological health through the gut-brain axis.
The therapeutic qualities of specific probiotic strains, such as L. acidophilus, include immunomodulation, which can have osteoprotective effects and may influence the balance of Treg-Th17 cells. This highlights the potential for targeted probiotic interventions in managing autism spectrum disorders.
Interplay Between Nutrition and Immunity
The intricate dance between nutrition and immunity within the gut ecosystem plays a pivotal role in maintaining health and combating disease. Probiotics and prebiotics, key players in this ballet, modulate the immune system by influencing cellular metabolism and epithelial barrier functions. Early colonization by beneficial microbes such as Bacteroides and Bifidobacterium species is crucial for immunological control, highlighting the dynamic nature of the gut microbiome.
The gut microbiome's development is significantly shaped by a mother's diet, emphasizing the importance of nutritional choices in establishing a robust immune system.
Understanding the effects of nutrition on immunity involves unraveling the complex interactions between gut microbiota, metabolites, and the host's immune responses. Short chain fatty acids (SCFAs), for example, are metabolites with a profound impact on appetite regulation and energy homeostasis, further illustrating the gut's influence on overall well-being.
- Influence on Immune System: Probiotics and prebiotics affect cellular metabolism and proliferation.
- Epithelial Barrier Functions: These substances help maintain the integrity of the gut lining.
- Immunological Control: Early microbial colonization is essential for developing immune regulation.
- Metabolite Impact: SCFAs play a role in appetite and energy balance, affecting immune health.
Emerging Research on Microbiome and Autism
Recent Studies and Findings
Emerging research in the microbiome's role in autism spectrum disorders (ASD) has unveiled complex interactions between gut bacteria and neurological development. Recent studies highlight the need for larger sample sizes and longitudinal designs to better understand these connections. Variations in diet and gastrointestinal symptoms add layers of complexity to the data.
Multi-omics technologies are at the forefront, aiming to dissect the functional contributions of gut microbiota to brain development and behavior. The interplay between microbial composition, metabolites, and immune markers is under intense scrutiny, with a focus on how dietary and microbial interventions can restore gut balance and improve behavioral outcomes.
The pursuit of gut eubiosis through targeted interventions holds promise for therapeutic advances in ASD.
Despite the progress, gaps remain. The call for more randomized, controlled clinical trials is clear, especially for adolescents and adults with ASD. The health benefits and limitations of biotics, including probiotics and prebiotics, are yet to be fully understood, necessitating further exploration in this burgeoning field.
Potential Biomarkers for Autism
The quest for biomarkers in autism spectrum disorders (ASD) is gaining momentum, with recent studies highlighting the potential of certain immune and gut-related indicators. Elevated plasma cytokines have emerged as a promising area of focus. These cytokines, including IL-1\u03b2, IL-6, IL-8, and IL-12p40, are not just bystanders; they are actively associated with more abnormal behavior in children with autism, suggesting a direct link to ASD symptomatology.
The interplay between the immune system and gut microbiota is intricate, and disruptions can manifest in the central nervous system, affecting behavior and cognitive functions.
Identifying these biomarkers is not just about diagnosis; it's about opening doors to personalized treatment strategies. Here's a snapshot of the biomarkers under investigation:
- Immune markers: Elevated cytokines and evidence of immune dysfunction
- Gut-related markers: Changes in gut microbiota composition
- Metabolic markers: Abnormal levels of certain metabolites
The potential of these biomarkers lies in their ability to reflect the underlying pathophysiology of ASD and guide interventions. As research progresses, these indicators may help tailor treatments to the individual, improving outcomes and quality of life for those on the autism spectrum.
Future Directions in Microbiome Research
As we look to the future, the exploration of the gut microbiome in relation to autism spectrum disorders (ASD) is poised for groundbreaking advancements. The integration of big data analytics and machine learning promises to unravel the complex interactions between gut microbes and neurological development. Researchers are particularly interested in how these insights could lead to personalized medicine approaches for ASD.
Emerging technologies are set to revolutionize our understanding of the microbiome's role in autism. For instance, next-generation sequencing and bioinformatics will enable the identification of novel microbial species and their functions. This could pave the way for the development of new probiotic strains specifically tailored to modulate the gut-brain axis in autism.
- Identification of novel microbial species
- Understanding microbial functions
- Development of targeted probiotic strains
The quest for biomarkers that can predict the efficacy of probiotic treatments in ASD is another exciting avenue. These biomarkers would not only assist in treatment customization but also in monitoring the long-term success of interventions.
With the rapid pace of research, the coming years will undoubtedly witness a surge in studies focusing on the intricate relationship between the gut microbiome and autism. The ultimate goal is to enhance the quality of life for individuals with ASD through innovative and effective therapies.
Conclusion
The exploration of the gut microbiome's role in autism spectrum disorder (ASD) has unveiled significant insights into how gut health may influence neurological conditions. The evidence suggests that children with autism often experience gut dysbiosis, which can manifest in gastrointestinal symptoms and potentially impact behavior and cognitive functions. While the research on probiotics and fecal microbiota transplantation (FMT) shows promise in alleviating some of these symptoms and improving the quality of life for individuals with ASD, the field is still in its infancy. It is crucial to approach these findings with cautious optimism, recognizing the need for further studies to establish standardized treatments, understand the long-term effects, and unravel the complex interactions between the gut microbiome and the brain. Ultimately, a better grasp of these relationships could lead to more effective interventions and support for those living with autism.
Frequently Asked Questions
What is the gut-brain axis and how does it relate to autism?
The gut-brain axis refers to the complex communication network between the gastrointestinal tract and the brain. In autism, research suggests that alterations in gut microbiota can impact neurological development and behavior, potentially influencing the severity of autism symptoms.
How does the gut microbiome affect children with autism?
Children with autism often exhibit imbalances in the gut microbiome, which can lead to inflammation, immune dysfunction, and the production of metabolites that may negatively affect the central nervous system and contribute to the symptoms of autism.
Can probiotics improve gastrointestinal symptoms in children with autism?
Yes, studies have shown that probiotic supplementation can improve gastrointestinal symptoms in children with autism, which may also correlate with a reduction in autism severity.
What role does stool testing play in managing gut health in autism?
Stool testing provides insights into the composition of the gut microbiome, helping to identify microbial imbalances and assess the effectiveness of dietary interventions and probiotic treatments in children with autism.
Are gluten-free and casein-free diets beneficial for gut health in children with autism?
Some observational studies suggest that a gluten-free and casein-free diet may alleviate gastrointestinal problems and improve behavioral traits in children with autism, though individual responses can vary.
What is fecal microbiota transplantation (FMT) and how is it used in autism?
FMT involves the transfer of stool from a healthy donor to the gastrointestinal tract of an individual with autism, with the aim of restoring a healthy microbiome balance. Clinical trials have explored its impact on behavioral and inflammatory responses in autism.
How does the immune system interact with gut health and autism?
The immune system, particularly autoimmunity and inflammation, plays a significant role in gastrointestinal dysfunction in autism. Probiotics may help modulate immune responses and improve gut health in children with autism.
What recent research has been conducted on the microbiome and autism?
Recent studies have focused on the dysbiosis of the gut microbiome in autism, the effects of probiotic treatments, and the identification of potential biomarkers for autism, aiming to advance our understanding and treatment of the condition.
On This Page
Frequently asked questions
How does gut health influence behaviors and symptoms in autism?
What role do probiotics play in supporting autism gut health?
How can stool testing help in understanding gut microbiome imbalances in autism?
What are some gentle ways to support the gut-brain connection in autistic individuals?
Are there sensory-friendly products, like calming blankets or autism-themed apparel, that can support comfort while managing gut health?
How do dietary changes, such as gluten-free or casein-free diets, impact gut health and autism symptoms?
What should families know about the safety and long-term effects of fecal microbiota transplantation (FMT) in autism?
How can autism disability support services incorporate gut health awareness into their care plans?
Can sensory tools or Autism-themed decor help create a supportive environment that complements gut health interventions?

About the HeyASD.com Team
Autistic‑owned • Values‑led • Sensory‑friendly design
We are autistic creators, writers, and advocates dedicated to producing resources that are practical, sensory-aware, and grounded in lived experience. Our mission is to make information and products that support the autistic community accessible to everyone, without jargon or condescension. Learn more about our team.
This article is written from lived autistic experience and an evidence-aware perspective. It is for general informational purposes only and should not be taken as medical, legal or therapeutic advice.
Always consult a qualified clinician or occupational therapist for individual needs and circumstances.

About Our ASD Blog
HeyASD is more than a store, it’s a calm, supportive space for autistic adults and the people who care about them. Explore identity-affirming stories, sensory regulation tools, and uplifting resources from our community.
Thank you for reading. We hope these resources bring comfort and clarity.