Nutrition for Individuals with Autism: A Guide

Written by HeyASD.com Team
On This Page
Frequently asked questions
How can I create a sensory-friendly diet that supports my unique needs?
What are some simple tips for autism meal planning that reduce stress?
How does nutrition impact behavior and focus in autistic individuals?
Are there specific nutrients that are especially important for disability support nutrition?
What types of comfortable clothing or calming blankets can help during mealtime?
How can I introduce new foods without overwhelming sensory sensitivities?
What role does healthy eating play in managing common autism-related health concerns?
How can caregivers support balanced nutrition while respecting sensory preferences?
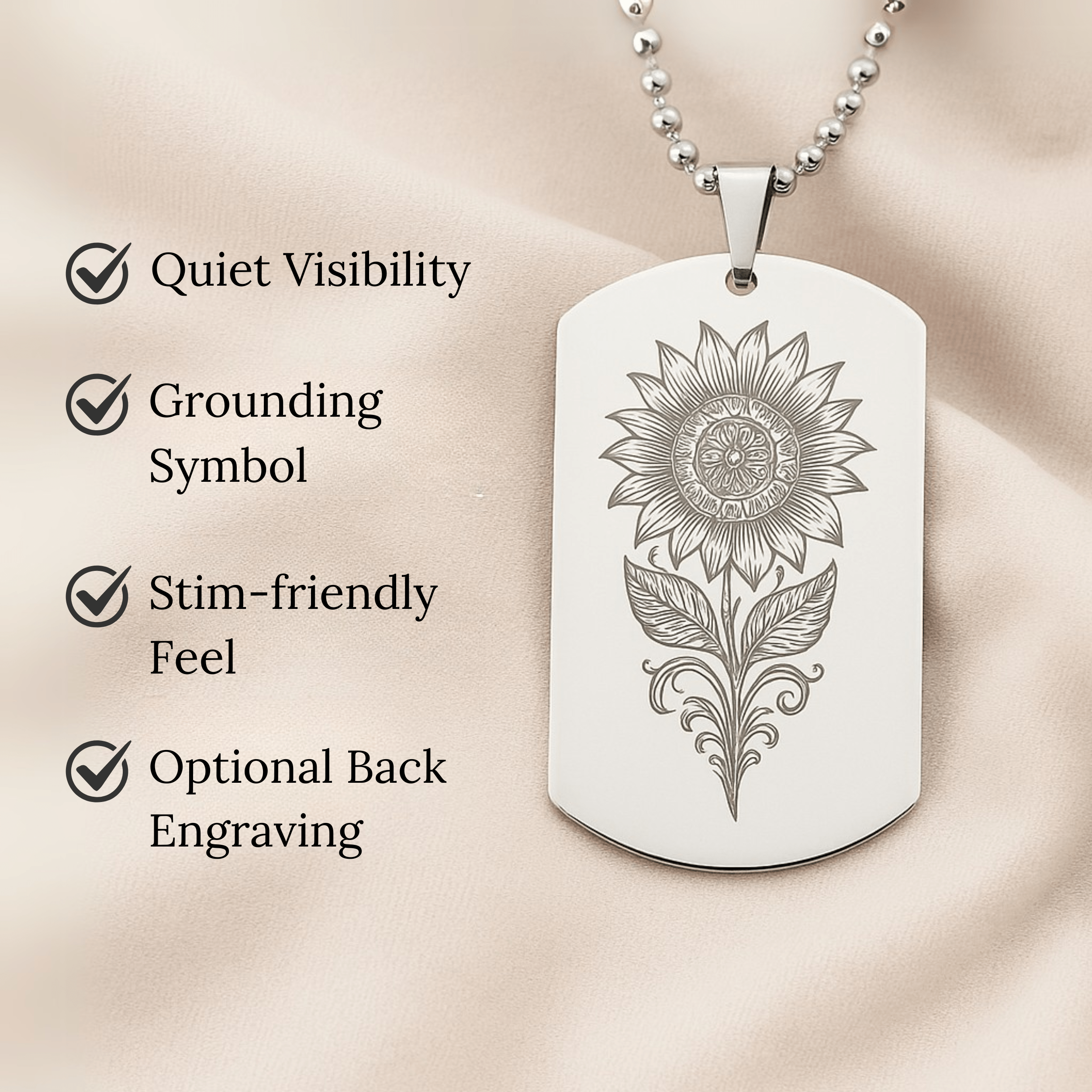
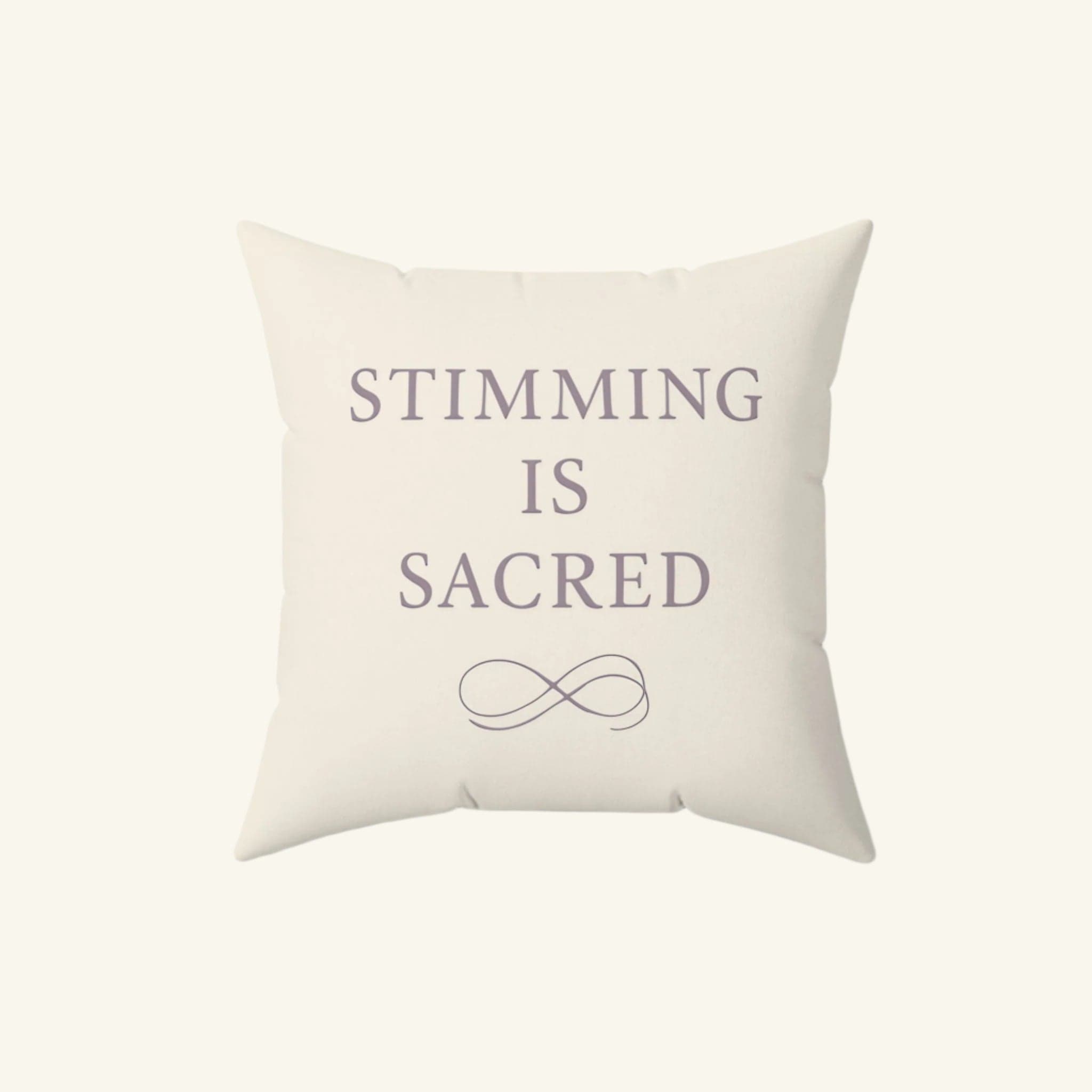
Are there sensory tools or Autism-themed decor that create a calming eating environment?

About the HeyASD.com Team
Autistic‑owned • Values‑led • Sensory‑friendly design
We are autistic creators, writers, and advocates dedicated to producing resources that are practical, sensory-aware, and grounded in lived experience. Our mission is to make information and products that support the autistic community accessible to everyone, without jargon or condescension. Learn more about our team.
This article is written from lived autistic experience and an evidence-aware perspective. It is for general informational purposes only and should not be taken as medical, legal or therapeutic advice.
Always consult a qualified clinician or occupational therapist for individual needs and circumstances.

About Our ASD Blog
HeyASD is more than a store, it’s a calm, supportive space for autistic adults and the people who care about them. Explore identity-affirming stories, sensory regulation tools, and uplifting resources from our community.
Thank you for reading. We hope these resources bring comfort and clarity.